Introduction
Atopic dermatitis is a chronic inflammatory skin condition that affects up to one fifth of the population in developed countries.1 It is characterized by relapsing pruritic patches and plaques with exudation, crusting, scaling, fissures, and lichenification in later stages.2 Atopic dermatitis lesions may be intensely itchy and elicit discomfort. African Americans are disproportionately affected by atopic dermatitis compared to their Caucasian counterparts, 19.3% and 16.1%, respectively.3 Additionally, atopic dermatitis may be more severe in patients with skin of color and for non-Hispanic black and Hispanic children, is more likely to persist into adulthood.4 Atopic dermatitis in skin of color patients may be particularly distressing due to post-inflammatory hyperpigmentation, which often leads to psychosocial effects and negative impacts on quality of life and productivity.5 In vivo, atopic dermatitis is active in both lesional and non-lesional skin.6 We highlight a case in which treating atopic dermatitis aggressively in a patient of African descent not only leads to clinically improved areas of atopic dermatitis and post-inflammatory hyperpigmentation, but also improves hyperpigmentation in non-lesional skin.
Case Presentation
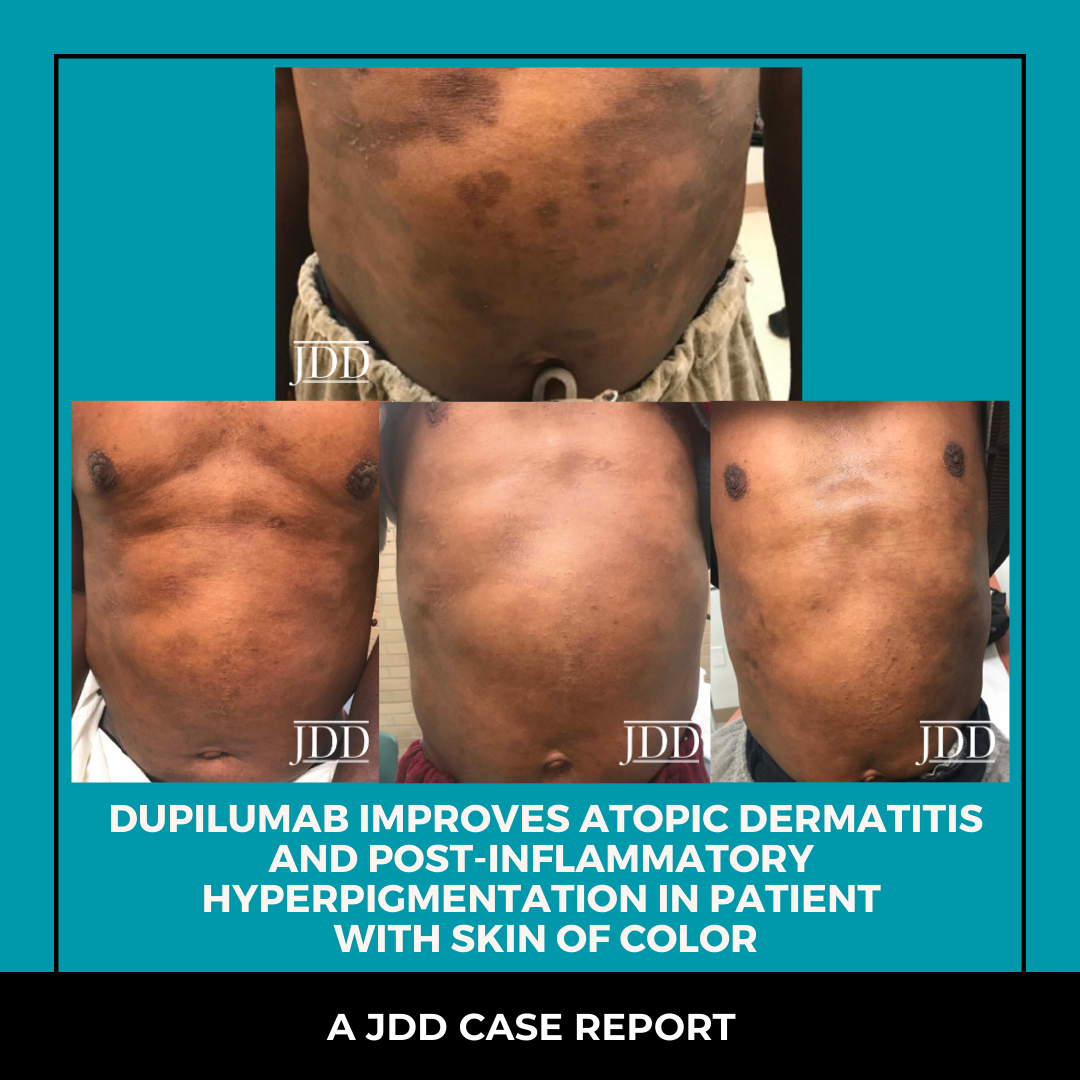
A 53-year-old male of African-descent presented with a 1-year history of worsening pruritic rash. He was applying petroleum jelly without relief. Past medical history was significant for deaf-ness and iron deficiency. On physical exam, there were multiple hyperpigmented plaques, hyperpigmented lichenified plaques, and hyperpigmented patches on the trunk, extremities, buttocks, neck, and face. The patient was diagnosed with moderate-se-vere atopic dermatitis. Triamcinolone ointment 0.1%, tacrolimus 1% and cetirizine 20 mg po daily were prescribed. Gentle skin care and soak and smear technique were reviewed. Two months later, the patient received 600 mg loading dose of dupilumab. Two weeks later, the patient’s atopic dermatitis and pruritus were improved (Figure 1). The patient continued 200 mg sub-cutaneous every 2 weeks resulting in continued improvement of atopic dermatitis, post-inflammatory hyperpigmentation, and apparent hyperpigmentation in non-lesional areas (Figures 2 and 3). Gentle skin care routine emphasized with intermittent use of topical triamcinolone 0.1% ointment or tacrolimus 1% ointment as needed for pruritus. After completion of the fifth month, his next 200 mg injection was performed at the 3-week mark instead of the 2-week mark. His atopic dermatitis flared during this time with pruritus. Dupilumab frequency was re-instated at every 2 weeks. The atopic dermatitis flare resolved, and post-inflammatory hyperpigmentation improved (Figure 4).

FIGURE 1. Improvement of atopic dermatitis two weeks following initiation of dupilumab.

FIGURES 2 AND 3. Continued improvement of atopic dermatitis, post-inflammatory hyperpigmentation and apparent hyperpigmentation in non-lesional areas.

FIGURE 4. Resolution of atopic dermatitis flare and improved post-inflammatory hyperpigmentation.
Discussion
Atopic dermatitis and post-inflammatory hyperpigmentation are among the top five most common chief complaints seen by dermatologists in skin of color patients. A study conducted on patients that presented to the Skin of Color Center at St. Luke’s-Roosevelt Hospital Center in New York, NY found dyschromias, including post-inflammatory hyperpigmentation, to be the second most common diagnosis in African-American patients, while it was not even among the top ten diagnoses in Caucasian patients.7 Atopic dermatitis often leads to post-inflammatory pigment alteration, most commonly post-inflammatory hyperpigmentation, in those with skin of color.8 Chronic inflammation results in increased melanocyte density, hyperplasia, and hypertrophy.9 This strongly suggests increased function of melanocytes and explains why inflammatory conditions such as atopic dermatitis cause hyperpigmentation. Post-inflammatory hyperpigmentation tends to be more persistent and clinically visible in patients with darker skin tones.10
Dupilumab is a monoclonal antibody that blocks the IL-4 alpha receptor and therefore inhibits IL-4 and IL-13 signaling, preventing the release of type 2 cytokines that promote inflammation in atopic dermatitis.11 A randomized control trial of 54 patients treated with dupilumab resulted in reduced cellular in-filtrates and significant clinical improvement.11 After 16 weeks of treatment, researchers observed reversal of lesional atopic dermatitis phenotype.11
In this case, the post-inflammatory hyperpigmentation was quite severe. After initiation of dupilumab, clinical improvement of the post-inflammatory hyperpigmentation, and lightening of overall skin tone was noted. Suarez et al. compared chronic atopic dermatitis lesional skin, non-lesional skin, and normal skin biopsies and found that non-lesional skin has cutaneous T-cell expansion.6 Non-lesional and lesional skin differ from normal skin in regards to keratinocyte terminal differentiation and inflammatory pathways.6 The abnormalities seen in lesional atopic dermatitis skin are also seen in non-lesional skin, which suggests that the total body surface area of skin in patients with atopic dermatitis is abnormal, even if it appears normal clinically.6 This is especially important in skin of color patients who are more prone to residual effects of atopic dermatitis such as post-inflammatory hyperpigmentation.
Systemically treating moderate-severe atopic dermatitis with dupilumab in skin of color patients with significant, distressing hyperpigmentation should be considered. Reducing hyperpig-mentation in non-clinically apparent areas of atopic dermatitis and evident post-inflammatory hyperpigmentation areas may contribute positively to quality of life. For skin of color patients, aggressive treatment with duplimab may accelerate the return of the patient’s overall normal skin tone.
Post-inflammatory hyperpigmentation often comes with psy-chosocial impairments. A study assessing quality of life found that patients with atopic dermatitis reported significantly more mood and sleep disorders compared to controls.5 These patients had significantly reduced health related quality of life on physical and mental domains.5 In a study of 419 patients, those with post-inflammatory hyperpigmentation had higher scores on the Dermatology Life Quality Index (DLQI) survey, which indicates poorer quality of life, when compared to patients with other disorders of hyperpigmentation.12 Additionally, the study demonstrated that DLQI scores were higher in women and those younger than 35 years of age. Having a graduate level education was associated with significantly lower DLQI scores, showing that patients with lower education level had a more negative impact on quality of life.12 Atopic dermatitis is a systemic disease. Dupilumab’s impact on post-inflammatory hyperpigmentation and apparent hyperpigmentation in non-lesional skin empha-sizes the scientific data of atopic dermatitis activity in lesional and non-lesional skin. When considering whether to treat atop-ic dermatitis aggressively, it is essential to consider the overall impact of the disease including the psychosocial burden, subse-quent post-inflammatory hyperpigmentation and in some cases overall skin hyperpigmentation. Patients with atopic dermatitis experience higher rates of anxiety, depression, sleep disorders, and decreased work productivity.5 Additionally, the resulting post-inflammatory hyperpigmentation can negatively impact quality of life. The burden of atopic dermatitis in patients with skin of color goes way beyond pruritus. In our case, aggressive treatment with dupilumab resulted in improvement of the ap-parent hyperpigmentation in clinically non-lesional skin (but likely scientifically lesional skin), post-inflammatory hyperpigmentation and atopic dermatitis.
Disclosures
There are no potential perceived conflicts of interest and/or sup-port, financial interests, or patents for Ciara Grayson.
Dr. Heath is a consultant for Sanofi-Regeneron and Pfizer.
References
Originally published in the Journal of Drugs in Dermatology in July 2020.
Grayson, C., & Heath, C. R. (2020). Dupilumab Improves Atopic Dermatitis and Post-Inflammatory Hyperpigmentation in Patient With Skin of Color. Journal of drugs in dermatology: JDD, 19(7), 776-778.
https://jddonline.com/articles/dermatology/S1545961620P0776X
Content and images republished with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
The Journal of Drugs in Dermatology is available complimentary to US dermatologists, US dermatology residents, and US dermatology NP/PA. Create an account on JDDonline.com and access over 15 years of PubMed/MEDLINE archived content.
Did you enjoy this case report? You can find more here.
