Hosted by George Washington University, in Partnership with ODAC Dermatology, Aesthetic & Surgical Conference and Next Steps in Derm
Even during a global pandemic we cannot forget that Acne Vulgaris is one of if not THE most common skin condition afflicting our patients and the general populace. With the disruption of clinics and conferences, innovative vehicles for the dissemination of the most up to date data and expert anecdote are certainly and sorely needed.
Enter the GW Virtual Acne Appraisal Conference: A 3 hour program that promises to pander to your pimple popping practices with short but sweet lectures from the acne gurus covering the gamut of the big A. From treatments to treats, from considering the microbiome to unique treatment approaches in specific patient populations, we will cover it all. And if that wasn’t enough, we will round it out with a perusal of the therapeutic pipeline. It will be all that and a bag of chips (which may or may not cause acne…you need to tune in to find out).
Agenda
8:00 – 8:15 – Introduction and Welcome
8:15 – Topical Management of Acne– James Q. Del Rosso, DO, FAOCD, FAAD
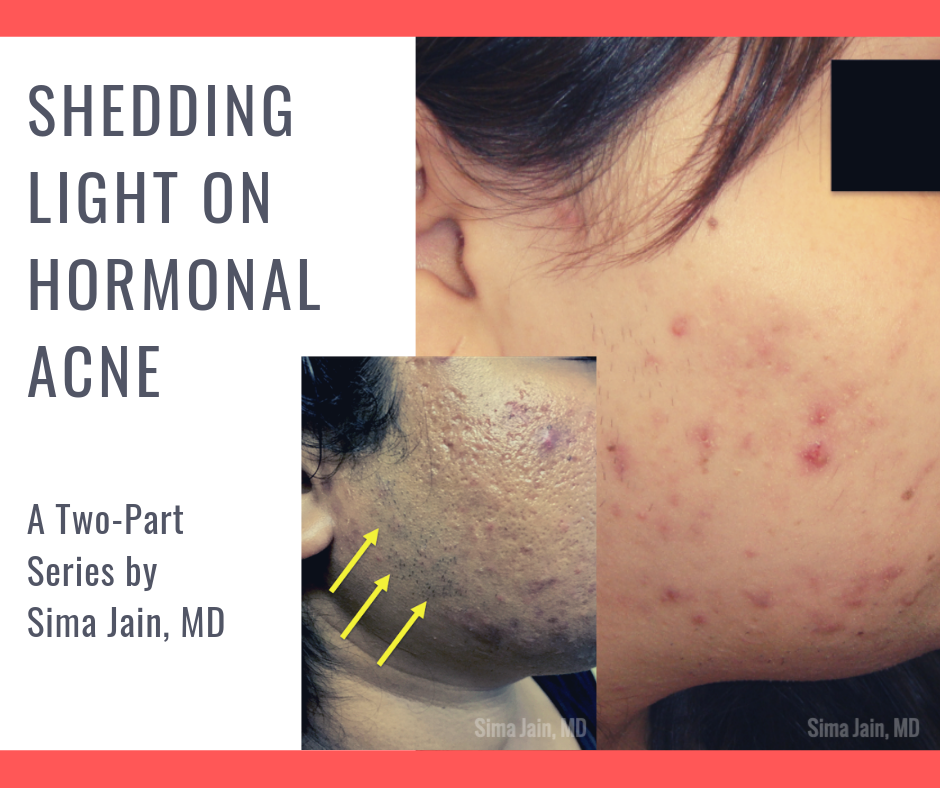
8:30 – Use of Hormonal Therapies in Acne– Julie Harper, MD
8:50 – Use of Antibiotics in Acne – Neal Bhatia, MD
9:10 – Issues with Isotretinoin: Fact vs. Fiction – Jenna C. Lester, MD
9:30 – Microbiome Manipulation for the Management of Acne – Adam Friedman, MD, FAAD
9:45 – Diet and Alternative Therapies: What to know for Acne management – Vivian Shi, MD
10:00 – Management Considerations for Skin of Color Patients with Acne –Andrew Alexis, MD, MPH
10:20 – Managing Acne in the LGBTQ+ Population – Angelo Landriscina, MD
10:40 – New and Emerging Therapies for Acne – Leon Kircik, MD