There is both science and strategy behind movie coming attractions: Hook the audience with some but not all of the most enticing morsels without spoiling the meal. The same could technically be said about the ODAC Virtual Pre-Conference Symposium, though, biased we may be, it is truly the kick off to ODAC educational greatness. Now in its third year, this interactive case-based program covers a cornucopia of complex topics is coming back with all new faculty and cases. Set your microwave to “pop,” prep a licorice straw for your 48 oz beverage, and enjoy the show with moderator and ODAC Co-Chair Dr. Adam Friedman and esteemed faculty.
Tuesday, November 15th | 5:30 – 7:30 PM ET
Part 1 | 5:30 PM – 6:30 PM ET
Welcome & Introductions with Adam Friedman, MD, FAAD
Challenging Cases of Alopecia with Michelle Oboite, MD
Challenging Cases of Vitiligo with David Rosmarin, MD
Live Audience Q&A
Part II | 6:30 – 7:30 PM ET
Welcome & Introductions with Adam Friedman, MD, FAAD
Atopic Dermatitis in Pediatric Patients with Kaiane Habeshian, MD
Bad Ulcers: When it’s NOT Pyoderma Gangrenosum with Olayemi Sokumbi, MD
Live Audience Q&A
Pre-Con Concludes | 9:00 PM ET
ODAC Dermatology, Aesthetic & Surgical Conference is the premier clinical CE dermatology conference expertly curated to provide comprehensive, annual updates and fresh practical pearls in medical, aesthetic and surgical dermatology. Elite faculty provide four days of cutting edge lectures, Q&A, live demonstrations and workshops for today’s dermatology provider.
Attend ODAC to stay informed and up-to-date on clinical dermatology updates, new treatments, new uses for old treatments, new product lines, changes to therapeutic guidelines and to witness live demonstrations from the experts. Unique to ODAC, each presentation focuses on practical pearls you can immediately use in your practice.
ODAC 2023 registration is now open! The event will be held January 13 – 15, 2023 at the JW Marriott Grande Lakes in Orlando, Florida. Register today: https://orlandoderm.org/registration/

The 2022 ODAC Dermatology, Aesthetic & Surgical Conference took place January 14 – 17, 2022 at the Rosen Shingle Creek in Orlando, Florida. Below is a current conference coverage recap. Additional articles will be added and available soon.
Source: MDedge
Source: MDedge
Source: Practical Dermatology

NEW YORK, Jan. 25, 2022 /PRNewswire/ — WebMD Health Corp., an Internet Brands company and a leader in health information services for physicians, other healthcare professionals and consumers, today announced that it has acquired SanovaWorks, a global multiplatform company focused on delivering targeted educational offerings and learning solutions for dermatologists.
Sanovaworks hosts leading medical conferences ODAC Dermatology, Aesthetics and Surgical and Skin of Color and offers web-based learning tools, publications such as Journal of Drugs in Dermatology (JDD) and virtual webinar and podcast series. In addition, SanovaWorks offers the online and audio-format Derm in Review, a board certification and recertification course.
The acquisition builds on the core competencies of WebMD’s MedscapeLIVE, Medscape’s market leading experiential business providing impactful in-person and virtual opportunities for healthcare professionals (HCPs) to congregate, learn and share. MedscapeLIVE offers proprietary live conferences, peer-to-peer webinars, symposia and various other educational engagement programs.
“The addition of SanovaWorks deepens WebMD’s commitment to providing high-quality, engaging experiences for HCPs with an expanded offering to dermatologists, one of our largest professional communities,” said Ann Bilyew, Internet Brands Senior Vice President, Health and WebMD Group General Manager, Provider Services. “With SanovaWorks, we build on MedscapeLIVE’s innovative learning solutions with expansive and relevant content that supports dermatologists throughout their careers, while providing additional opportunities to reach this important audience for sponsors and supporters.”
“SanovaWorks shares WebMD’s core mission to continually meet the educational needs of clinicians with the information and content they need, when and where they need it,” said Shelley Tanner, CEO of Sanovaworks. “The extensive reach of MedscapeLIVE with dermatology professionals worldwide enables us to have an even greater impact, particularly as their need for timely, relevant learnings grows.”
Terms of the acquisition were not disclosed.
About SanovaWorks
SanovaWorks is a healthcare communications company with more than 20 years of experience in the creation and dissemination of educational resources in dermatology, aesthetics and beyond. Reaching over 100,000 worldwide dermatology professionals monthly, SanovaWorks is a trusted healthcare communication source that produces the Journal of Drugs in Dermatology (JDD), ODAC Dermatology, Aesthetic and Surgical Conference, Skin of Color Update, Next Steps in Dermatology, Dermatology In-Review and the newly released Atlas in Dermatology. For more information, please visit sanovaworks.com.
About WebMD Health Corp.
WebMD, an Internet Brands company, is at the heart of the digital health revolution that is transforming the healthcare experience for consumers, patients, healthcare professionals, employers, health plans and health systems. Through public and private online portals, mobile platforms, and health-focused publications, WebMD delivers leading-edge content and digital services that enable and improve decision-making, support and motivate health actions, streamline and simplify the healthcare journey, and improve patient care.
The WebMD Health Network includes WebMD Health, Medscape, Jobson Healthcare Information, MediQuality, Frontline, Vitals Consumer Services, Aptus Health, Krames, PulsePoint, The Wellness Network, MedicineNet, eMedicineHealth, RxList, OnHealth, Medscape Education, and other owned WebMD sites. WebMD®, Medscape®, CME Circle®, Medpulse®, eMedicine®, MedicineNet®, theheart.org® and RxList® are among the trademarks of WebMD Health Corp. or its subsidiaries.
About Internet Brands
Headquartered in El Segundo, Calif, Internet Brands® is a fully integrated online media and software services organization focused on four high-value vertical categories: Health, Automotive, Legal, and Home/Travel. The company’s award-winning consumer websites lead their categories and serve more than 250 million monthly visitors, while a full range of web presence offerings has established deep, long-term relationships with SMB and enterprise clients. Internet Brands’ powerful, proprietary operating platform provides the flexibility and scalability to fuel the company’s continued growth. Internet Brands is a portfolio company of KKR and Temasek. For more information, please visit www.internetbrands.com.
Shannon Miller, 7 time Olympic medalist and leader of the 1996 Magnificent 7, will give the keynote address at the ODAC Dermatology, Aesthetic & Surgical Conference (ODAC). The address, “Gold Medal Mindset with Shannon Miller: Motivation, Teamwork & Commitment to Excellence,” will be given Friday, January 14, at 6:30 p.m. at the Rosen Shingle Creek in Orlando.
Shannon will discuss how the gold medal mindset not only helped her win seven Olympic medals, but also battle cancer, and how these lessons continue to help her through the day-to-day effort of finding that illusive work-life balance. Shannon will share what it takes to succeed: the importance of goal setting, teamwork, positive attitude and resiliency.
“We are honored to have Shannon share her story of overcoming personal challenges, which can be an inspiration to us all,” said Shelley Tanner, CEO and president of SanovaWorks, which produces ODAC. “Shannon serves as the inaugural keynote speaker in recognition of our 20th ODAC. We look forward to developing a long tradition of keynote addresses that inspire and encourage for the year ahead.”


ODAC provides pearls and clinical updates in medical, aesthetic and surgical dermatology through an engaging learning experience, including live demonstrations, panel discussions and audience Q&As. ODAC historically attracts nearly 700 dermatology physicians, residents, nurse practitioners and physician assistants each year. Up to 26.25 AMA PRA Category 1 Credits™ are available. The conference runs from January 14 through January 17.
ODAC is a product of SanovaWorks, publisher of the Journal of Drugs in Dermatology (JDD) and producer of the Skin of Color Update conference.
Registration is available at orlandoderm.org.
Tuesday, October 26th, 2021 | 7:00 – 8:00 PM ET
Active ingredients play a critical role in the efficacy and safety of cosmeceuticals. Join Dr. Zoe Draelos, as she shares information on cosmeceutical ingredients. This presentation will include information on the mechanisms of action and benefits for various skin conditions and concerns for ingredients found in SkinCeuticals products.
Speaker
Zoe Diana Draelos, MD
Dermatology Consulting Services, PLLC
PRODUCT GIVEAWAY
US Dermatology healthcare providers who attend the entire webinar will receive one full-sized item from the SkinCeuticals portfolio of skin care products. Products will be distributed by SkinCeuticals based on current inventory. Requests for specific products will not be taken. Shipments will be fulfilled in approximately six to eight weeks following the webinar. This program is only open to US Dermatology healthcare providers. PLEASE BE SURE TO REGISTER WITH THE ADDRESS YOU WOULD LIKE THE PRODUCT SHIPPED TO. ADDRESS CHANGES WILL NOT BE ACCEPTED. For questions about the product giveaway, please contact [email protected].
The virtual event is free and open to all healthcare practitioners, however, pre-registration is required.
Who doesn’t enjoy a little taste, a nibble to entice the educational appetite that will no doubt be satiated by ODAC 2022? No need to answer because we have your fix. The ODAC Virtual Pre-Conference Symposium will be a unique academic appetizer developed using audience feedback to provide the best and most clinically translatable experience for attendees (think mini hot dogs of conferences – if you know, you know). Join us for case based, literature distilling discussions on Acne, Psoriasis, Atopic Dermatitis, and Hidradenitis with experts from across the country. Tune in to digest the repartee between moderator and ODAC co-Chair Dr. Adam Friedman and esteemed faculty, all aimed at filling your clinical dermatology stomachs. Do not pass and make sure to come back for seconds.
5:30-5:35PM ET – Welcome & Introductions – Adam Friedman, MD, FAAD
5:35-5:55PM ET – Challenging Cases of Psoriasis – April W. Armstrong, MD, MPH
5:55-6:15PM ET – Challenging Cases of Acne – Jenna C. Lester, MD
6:15-6:30PM ET – Live Audience Q&A
6:30-7:30PM ET – Non-CME Product Theater Presentation Sponsored by Incyte – Atopic Dermatitis: The Burden of Disease & A Novel Topical Pathway – Adam Friedman, MD, FAAD
7:30-7:35PM ET – Welcome & Introductions – Adam Friedman, MD
7:35-7:55PM ET – Challenging Cases of Atopic Dermatitis – Jonathan Silverberg, MD, PhD, MPH
7:55-8:15PM ET – Challenging Cases of Hidradenitis Suppurativa – Ginette A. Okoye, MD, FAAD
8:15-8:30PM ET – Live Audience Q&A
Adam Friedman, MD, FAAD
April W. Armstrong, MD, MPH
Jenna C. Lester, MD
Ginette A. Okoye, MD, FAAD
Jonathan Silverberg, MD, PhD, MPH
Non-CME Product Theater Presentation Sponsored by Incyte
Atopic Dermatitis: The Burden of Disease & A Novel Topical Pathway
Adam Friedman, MD, FAAD
Presentation Sponsored By Incyte Dermatology
*This sponsored workshop is non-CE and will not be recorded.
CLAIMING CE
Creighton University Health Sciences Continuing Education designates this live activity for a maximum of 1.75 AMA PRA Category 1 Credit(s)™. In order to claim CE for this virtual symposium, you must be registered as a ODAC 2022 live attendee. Instructions on how to claim CE will be provided during the ODAC 2022 live event in Orlando, FL on January 14-17, 2022. You can register for ODAC 2022 here. (The sponsored workshop is non-CE.)
VIDEO RECORDING
The recording of the CE portion of this symposium will only be available to re-watch on the ODAC 2022 Onsite App. You must be a ODAC 2022 live attendee to access this platform. (The non-CE sponsored workshop will not be recorded.)
Psoriasis is a common autoimmune disorder with associated comorbidities that are more than skin deep. Patients with psoriasis are at increased risk for cardiovascular and metabolic disease, malignancies, and anxiety/depression. These patients suffer from a diminished quality of life; conversely, treatment of the disease can improve quality of life and reduce morbidity. Unfortunately, data indicate that patients with psoriasis do not receive optimal treatment, and that clinicians are not sufficiently equipped to select appropriate therapy from among the many new treatment options. The proposed educational initiative will provide clinicians with a solid foundation for understanding the pathophysiology of psoriasis along with other autoimmune diseases, how this pathophysiology informs treatment options, and the most recent clinical trial data for current and emerging agents and management recommendations available to guide therapy selection.
SPEAKER
Gary Goldenberg, MD
Assistant Clinical Professor, Dermatology
Mount Sinai School of Medicine
New York, NY
This webinar is hosted by ODAC.
This activity is provided by the University of Cincinnati.
Paradigm Medical Communications, LLC is the educational partner.
DISCLOSURE OF COMMERCIAL SUPPORT
This activity is supported by an educational grant from Bristol-Myers Squibb.
TARGET AUDIENCE
This initiative has been designed to address the educational needs of dermatology clinicians. It may also be of benefit to rheumatology and primary care clinicians, as well as other healthcare providers involved with or interested in the management of patients with psoriasis.
LEARNING OBJECTIVES
Upon proper completion of this activity, participants should be better able to:
– Identify the JAK/TYK2-STAT–mediated pathways involved in the pathophysiology of psoriasis
– Summarize evidence for the efficacy, safety, and mechanisms of action for new and emerging agents in psoriasis, and the implications for treatment
– Apply current research findings and recommendations to the treatment of psoriasis and comorbidities
AGENDA
– Pathophysiology of Psoriasis
– Recent Guidelines
– New Directions in Psoriasis Therapy: The Role of Recently Approved and Emerging Agents
– Tying it Together
ACCREDITATION INFORMATION
Physician Accreditation Statement
The University of Cincinnati is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
Physician Credit Designation Statement
The University of Cincinnati designates this live activity for a maximum of 1.0 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
PA Continuing Education
PAs may claim a maximum of 1.0 Category 1 credit for completing this activity. NCCPA accepts AMA PRA Category 1 Credit™ from organizations accredited by ACCME or a recognized state medical society.
Nurse Practitioner Continuing Education
The American Academy of Nurse Practitioners Certification Program (AANPCP) accepts certificates of participation for educational activities certified for AMA PRA Category 1 Credit™ from organizations accredited by the ACCME. Individuals are responsible for checking with the AANPCP for further guidelines.
For questions regarding CME credit, contact the Paradigm CME Department at (845) 398-5949 or [email protected].
STEERING COMMITTEE
April W. Armstrong, MD, MPH
Associate Dean, Clinical Research
Professor of Dermatology
Director, Clinical Research Support, Southern California CTSI
Keck School of Medicine
University of Southern California
Los Angeles, CA
Seemal R. Desai, MD, FAAD
Clinical Assistant Professor
Department of Dermatology
University of Texas Southwestern Medical Center
Dallas, TX
Gary Goldenberg, MD
Assistant Clinical Professor, Dermatology
Mount Sinai School of Medicine
New York, NY
DISCLOSURES
In accordance with ACCME requirements on disclosure, faculty and contributors are asked to disclose any relationships with commercial interests associated with the area of medicine featured in the activity. These relationships are described below. Any potential conflicts of interest have been resolved.
April W. Armstrong, MD MPH
Consulting Fees: Abbvie Inc; Bristol-Meyers Squibb Company; Dermavant Sciences Inc; Eli Lilly and Company; Janssen Pharmaceuticals, Inc; LEO Pharma Inc; Modernizing Medicine; Novartis; Ortho Dermatologics; Pfizer Inc; Regeneron Pharmaceuticals, Inc; Sanofi Genzyme; Sun Pharmaceutical Industries Ltd
Grant/Research Support: Abbvie Inc; Bristol-Meyers Squibb Company; Dermavant Sciences, Inc; Dermira; Eli Lilly and Company; Janssen Pharmaceuticals, Inc; Kyowa Kirin Pharmaceutical Research, Inc; LEO Pharma Inc; Novartis; Regeneron Pharmaceuticals Inc; Sanofi Genzyme; UCB Inc
Seemal R. Desai, MD, FAAD
Consulting Fees: Bristol-Myers Squibb Company; Pfizer Inc
Speakers Bureau: Pfizer Inc
Gary Goldenberg, MD
Consulting Fees: Abbvie Inc; Eli Lilly and Company; Pfizer Inc
Speakers Bureau: Abbvie Inc; Eli Lilly and Company; Pfizer Inc
University of Cincinnati staff members have no financial relationships to disclose.
Paradigm Medical Communications, LLC staff members have no financial relationships to disclose.
Independent peer, resident/fellow, and patient reviewers has no financial relationships to disclose.
RESOLUTION OF CONFLICT OF INTEREST
The University of Cincinnati has implemented a system to resolve conflicts of interest for each CME activity to help ensure content is objective, fair and balanced, independent, and aligned with the public interest. Conflicts, if any, are resolved through one or more processes. All CME content in this activity was independently reviewed to ensure that it is free of commercial bias, scientifically rigorous, aligned with the public interest, and compliant with all regulatory guidance and the ACCME’s Standards for Commercial Support of Continuing Medical Education.
DISCLOSURE OF UNLABELED USE
This educational activity may contain discussion of published and/or investigational uses of agents that are not approved by the FDA.
DISCLAIMER
This CME activity represents the views and opinions of the individual faculty, and does not constitute the opinion or endorsement of, or promotion by, Paradigm Medical Communications, LLC. Reasonable efforts have been taken to present educational subject matter in a balanced, unbiased fashion, and in compliance with regulatory requirements. However, each activity participant must always use his or her own personal and professional judgment when considering further application of this information, particularly as it may relate to patient diagnostic or treatment decisions including, without limitation, FDA-approved uses and any off-label uses.
If included, signed statements of informed consent granting permission for publication have been obtained for all photographs and videos in which an individual can be identified.
As an ACCME-accredited provider, Paradigm Medical Communications, LLC’s activities must include a balanced view of therapeutic options. Use of generic names contributes to this impartiality.
TERMS OF USE AND PRIVACY POLICY
Disclaimer
The materials provided for this activity are for informational purposes only, and should not be used for diagnosis or treatment of a health problem without consulting a licensed medical professional. This CME activity represents the views and opinions of the individual faculty, and does not constitute the opinion or endorsement of, or promotion by, Paradigm Medical Communications, LLC. References to any entity, product, service, or source of information on this website should not be considered an endorsement, either direct or implied, by Paradigm Medical Communications, LLC. Paradigm Medical Communications, LLC accepts no liability for the content referenced in this activity.
Privacy policy
Paradigm Medical Communications, LLC or hosted contracted partner is committed to protecting the privacy of those who participate in the activities located at www.paradigmmc.com (herein referred to as “website”). The information below describes the security of the website for safeguarding personal information and the rationale for collection and use of personal information.
Security/safeguarding personal information
This website has physical and procedural safeguards in place to prevent unauthorized access to personal information used to access this website.
Collection and use of your personal information
The submission of certain personally identifiable information is necessary to award and track the credits participants may earn after completing the program. Required items include first name, last name, degree, and email address. These items are necessary. Participants are also required to complete an evaluation of the CME activity. All evaluative information submitted is collected and retained, and used by Paradigm Medical Communications, LLC to continuously improve the learning experience.
Paradigm Medical Communications, LLC does not transfer, sell, or share personal information with outside parties. Paradigm Medical Communications, LLC will not otherwise disclose personal information unless required to in a legal process. Paradigm Medical Communications, LLC staff members review individual test results to the extent necessary to record and track participants’ credits.
CONTACT US
If you have any questions or comments, please email us at [email protected].
© 2020 Paradigm Medical Communications, LLC except where noted. Content may not be reproduced in whole or part without the express written permission of Paradigm Medical Communications, LLC.

New York (July 13, 2021) – The ODAC Dermatology, Aesthetic & Surgical Conference (ODAC) announced the appointment of Omar N. Qutub, MD, FAAD, to the position of director of equity, diversity and inclusion (EDI). Dr. Qutub is a medical and cosmetic dermatologist in private practice in Portland, Oregon. He will hold the position for the 2022 and 2023 conferences.
“We were impressed with Dr. Qutub’s innovative and impactful ideas for how to make ODAC more inclusive and diverse,” said Shelley Tanner, CEO and president of SanovaWorks, which produces ODAC. “Dr. Qutub’s passion for equity, inclusion and diversity in medicine is action-oriented and inspiring.”
In this role, Dr. Qutub will work closely with the ODAC Advisory Board and ODAC staff to promote the development and implementation of educational offerings aimed at improving cultural competence, diversity and equity within the field of dermatology. In addition, he will assist in creating a conference experience that is conducive to a collaborative learning environment that enhances professional development and advancement for all.
“With a focus on diversity and inclusion, I wholeheartedly believe that we can make strides as a specialty to serve all populations more proactively and thus more effectively,” said Dr. Qutub. “Serving as the director of EDI will invigorate what I view as a valuable aesthetic and medical training ground for young and experienced dermatologists alike.”
A graduate of Howard University College of Medicine, Dr. Qutub completed his dermatology residency at Howard University Hospital and the Veterans Affairs Medical Center in Washington, D.C. “At Howard, our mission was to serve the underserved, and to do so just as we would serve any other population; a lesson never once lost on me to this day,” said Dr. Qutub.
ODAC, which was founded in 2003, historically attracts nearly 800 dermatology physicians and allied health professionals each year. The 2022 event will take place January 14-17 at the Rosen Shingle Creek in Orlando. ODAC is a product of SanovaWorks, publisher of the Journal of Drugs in Dermatology (JDD) and producer of the Skin of Color Update conference.
###
Facial palsy is a common problem from which many patients do not completely recover and hence have to live with chronic sequelae.1 These may include discomfort, functional deficiencies, and aesthetic defects that can have significant physical and mental consequences and a detrimental impact on quality of life.2,3
Botulinum neurotoxin type A (BoNTA) is a key tool in the management of facial palsy, reducing associated synkinesis and hyperkinesis while also improving facial balance and overall aesthetics.1,4-6 Improvements in quality of life have also been demonstrated.1,7 Furthermore, BoNTA injection is minimally invasive and repeatable, and usually associated with few major adverse events;1,4,6 hence, BoNTA may be used as part of a long-term management strategy.
Standardized protocols are currently lacking for the use of BoNTA in patients with facial palsy.3,7 Owing to the great variety of clinical presentations, every case should be assessed and treated on an individual basis. Nonetheless, it is important for practitioners to achieve some degree of systematization within their overall methodology.
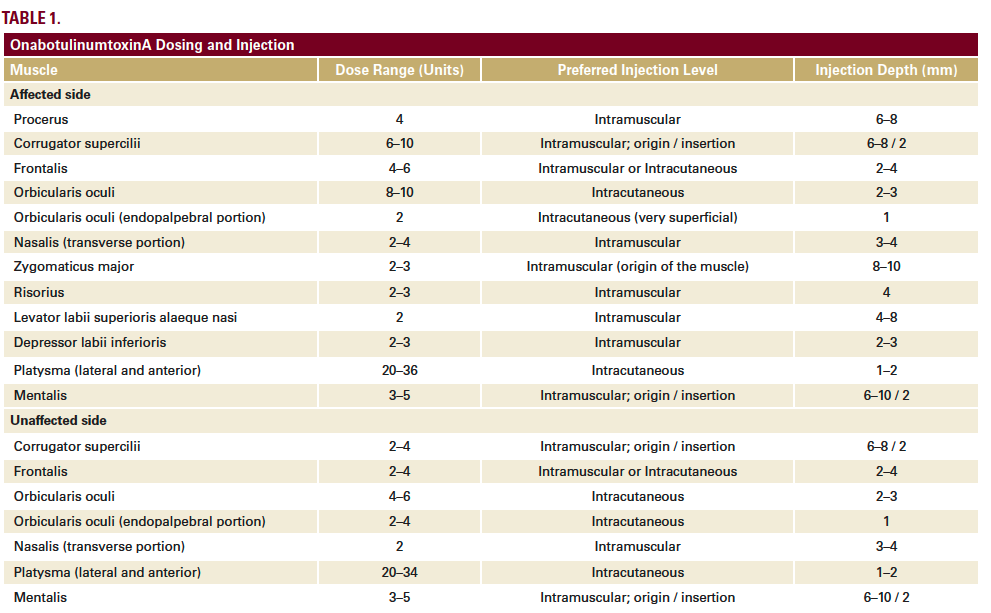
We have developed a full-face and neck approach to the treatment of facial palsy with BoNTA using standardized entry points, dose ranges and injection depths (Table 1). The overall focus is on:
• Treatment of both sides of the face to ameliorate synkinesis of the affected side, minimize hyperkinesis of the unaffected side, and improve overall facial symmetry.
• Treatment not just of the face but also both sides of the neck, with the aim of obtaining a progressive rejuvenation that minimizes the negative aesthetic effects of facial palsy.
Here, we present case studies of two patients with facial hemiparesis treated with BoNTA (onabotulinumtoxinA, Allergan, Dublin, Ireland) using this approach. The standard dilution was used for all treatments (50 units of onabotulinumtoxinA in 1.25 mL of saline solution).
A 53-year-old woman presented with left-side Bell’s palsy that had developed late in pregnancy when she was 40 years old. Routine blood testing and analyses for neurotropic viruses were negative. She was treated with corticosteroids until delivery.
Since then, she has had left facial hemispasm with painful tonic–clonic contractures, particularly in the lower face. Previous attempts at drug therapy with clonazepam, pregabalin, baclofen and gabapentin yielded only temporary and partial improvements. The addition of complementary treatments, such as B vitamins, physiotherapy, acupuncture and magnet therapy, had no benefit. She was also treated with BoNTA injections 2–3 times per year, primarily in the upper third with little treatment of the mid- and lower face; the neck was not injected. This approach was largely unsuccessful.
At 47 years of age, she underwent left retromastoid microcraniectomy to solve a vascular–nervous conflict at the origin of the left facial nerve in the bulb-pontin. After surgery, resolution of hemispasm was noted in the upper third of the face, with slight persistence in the middle third, but no change in the lower third. She was subsequently treated only with BoNTA on an irregular basis. The patient self-assessed the results using the 5-point Global Aesthetic Improvement Scale (GAIS): 1 = worsened; 2 = no change; 3 = improved; 4 = much improved; 5 = very much improved. Using this scale, the change was rated as a 3, representing an ‘improved’ appearance.
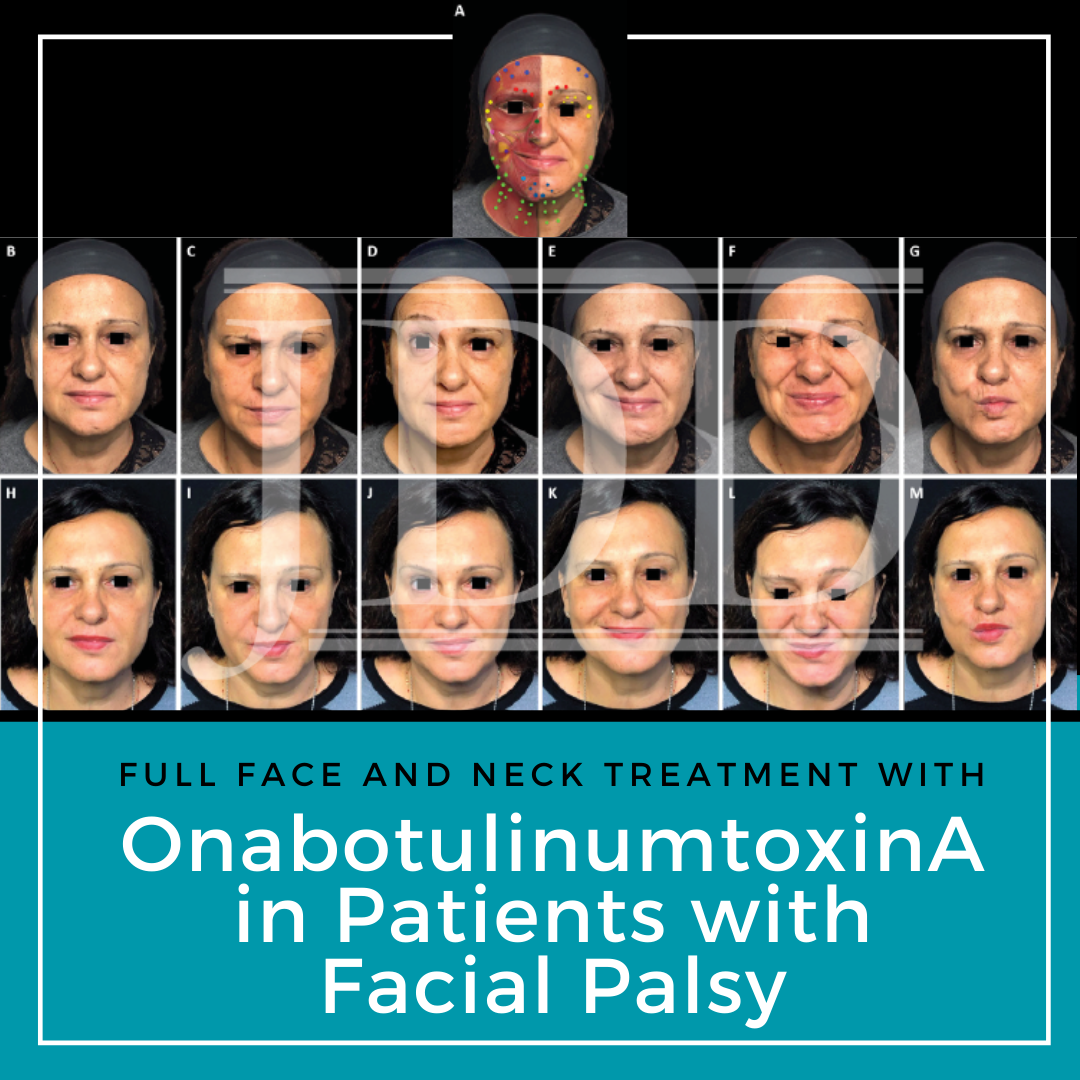
The patient began treatment at our center in April 2019, based on a full-face and neck approach using onabotulinumtoxinA (Table 2; Figure 1A). Repeat treatment using a similar injection pattern was undertaken in June 2019 and October 2019. Excellent results were achieved, as shown and described in Figure 1. Results on GAIS were assessed by the patient as a 5, representing a ‘very much improved’ appearance.

FIGURE 1. Full-face and neck treatment with onabotulinumtoxinA in a patient with facial palsy. A 53-year-old woman with left-side Bell’s palsy. Her injection plan with onabotulinumtoxinA is provided in (part A). She is also shown before (parts B–G) and 1 month after the first session of treatment (parts H–M). Notable features of the result include: good symmetrization, which was particularly evident in the eyebrows; relaxation of the chin area (which had been in constant contraction before treatment) and disappearance of synkinesis on the affected side; harmonization of the smile, with a reduction of hyperkinesis on the healthy side; maintenance of the ability to close her eyes despite treatment of the intrapalpebral portion of the orbicular muscle on the affected side; reduced platsymal contraction, which promoted a new aesthetic balance of facial contours; and general rejuvenation of the whole face, including the mandibular line. In part A: procerus, orange; corrugator supercilii, red; frontalis, mid-blue; orbicularis oculi, yellow; nasalis, dark green; zygomaticus major, pink; risorius, purple; depressor labii inferioris, pale blue; platysma, pale green; mentalis, dark blue.
A 68-year-old woman presented with post-surgical facial palsy on the left side, which had developed after excision of an acoustic nerve neurinoma at 45 years of age. For several months after surgery, she had to keep the eyelid on the paralyzed side closed with a plaster.
Passive physiotherapy yielded no improvement. After 6 months, she experienced spontaneous improvement and the eyelid resumed normal functionality.
At around 48–49 years of age, she began undergoing BoNTA treatment of the upper third of the healthy side of her face, with good aesthetic outcomes, self-assessed as a 4 (‘much improved’) on GAIS. Ten years later, she underwent a surgical neck lift with results that were initially positive but began to deteriorate within ~2 years.
The patient started treatment at our center in July 2019, based on a full-face and neck approach using onabotulinumtoxinA (Table 2; Figure 2A). Repeat treatment using a similar injection pattern was undertaken in December 2019 and May 2020. Excellent results were achieved (Figure 2), particularly considering her advanced age. The patient was especially satisfied with the improvements in the lower third, mouth, and neck areas. She assessed the overall results on GAIS as a 5, representing a ‘very much improved’ appearance.

FIGURE 2. Full-face and neck treatment with onabotulinumtoxinA in a patient with facial palsy. A 68-year-old woman post-surgical facial palsy on the left side. Her injection plan with onabotulinumtoxinA is provided in (part A). She is also shown before (parts B–F) and 1 month after the first session of treatment (parts G–K). Notable features of the result include: good symmetrization of the entire face; relaxation of the chin area and the eyebrow of the affected side (which had been in constant contraction before treatment) with associated disappearance of chin synkinesis and reduced upper eyelid synkinesis on the affected side; harmonization of the smile, with a reduction of hyperkinesis on the healthy side; maintenance of the ability to close her eyes despite treatment of the intrapalpebral portion of the orbicular muscle on the healthy side; and general rejuvenation of the whole face, including the mandibular line, chin and lips. In part A: procerus, orange; corrugator supercilii, red; frontalis, mid-blue; orbicularis oculi, yellow; nasalis, dark green; zygomaticus major, pink; risorius, purple; levator labii superioris alaeque nasi, cream; depressor labii inferioris, pale blue; platysma, pale green; mentalis, dark blue.
The approach employed in both patients involved injection of onabotulinumtoxinA into a wide variety of muscles on both sides of the face and neck. The total doses used (109–156 units per session) were substantially higher than in most previous facial palsy studies.4-6 This was because we did not limit ourselves to treating synkinesis, hyperkinesis and facial asymmetry, but also applied the principles of full-face aesthetic treatment8 to obtain an anti-aging, rejuvenating effect.
The two patients were treated differently according to individual functional alterations of the facial muscles, but the overall approach remained within our standardized framework (Table 1). In both cases, we have reported here on the treatment and outcomes across the first 3 sessions. These were given at intervals of 3–6 months, in line with the typical duration of effect of BoNTA, although there is evidence from previous studies of prolonged effects beyond 6 months in facial palsy.1 At each treatment session, patient photographs were captured in various projections both in static and dynamic pose. Results were verified at follow-up appointments 2–3 weeks after initial treatment. Touch-ups were given if necessary, typically to modulate the synkinesis that sometimes develops, particularly after treating the hyperactive (healthy) side of the face.
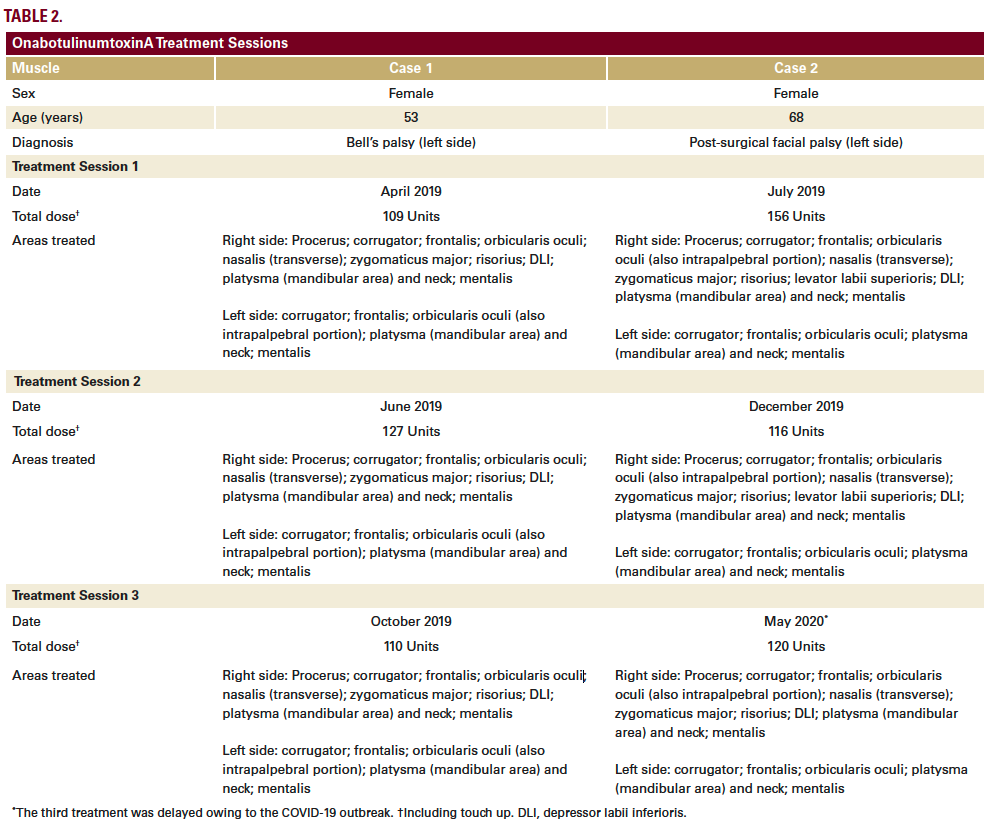
Both patients were extensively treated in the platysma to achieve a lifting and anti-aging effect within the lower third of the face. Normally, to obtain a lifting effect during non-palsy aesthetic treatment, we would reduce the action of the platysma, which has a depressive activity in its mandibular insertion, thereby fostering the antigravity effects of the muscles of the middle third of the face. In palsy cases, one side of the face has no active elevator muscles. Hence, it is even more important to reduce platysma activity, in order to rebalance asymmetric tissue descent.
Use of BoNTA across the whole face and neck is a minimally invasive approach to the aesthetic treatment of facial palsy with a low risk of major complications and the potential for excellent results. When treating these patients, it is essential to find a balance between the relaxing effects of BoNTA and preservation of residual motor function. If treatment is performed gradually by a skilled practitioner, an acceptable compromise between aesthetics and function can be achieved.
In the two cases described here, we have demonstrated marked improvements in synkinesis, hyperkinesis and facial symmetry, and also shown an anti-aging effect similar to that achieved with normal full-face treatments using BoNTA.8Results stabilized across multiple sessions of repeat treatment.
Content and images republished with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
The Journal of Drugs in Dermatology is available complimentary to US dermatologists, US dermatology residents, and US dermatology NP/PA. Create an account on JDDonline.com and access over 15 years of PubMed/MEDLINE archived content.
Did you enjoy this case report? You can find more here.

SanovaWorks has developed a partnership with and in support of Comprehensive Medical Mentoring Program. We are happy to announce that SanovaWorks will match the CMMP Medical Student Grant fund, which was started to help medical students from underrepresented populations with residency preparation expenses. This matching donation will ensure that more students are able to benefit from the grant. We join other partners in support of CMMP’s efforts of mentoring students, promoting diversity in medicine, and giving back to the communities.
Medical Students, Grants are Now Available for Residency Expenses
Comprehensive Medical Mentoring Program (CMMP) is aware that applying to residency can be a daunting process which can also become more stressful given the associated expenses that come with it.
CMMP is providing grants up to $1,000 for rising 4th-year minority medical students as they are preparing for away rotations and residency applications.
IF YOU ARE
JOIN US
SanovaWorks joins institutions that include George Washington University School of Medicine and Health Sciences, Howard University Hospital, Department of Dermatology, Georgetown University School of Medicine, and many others in support of CMMP.
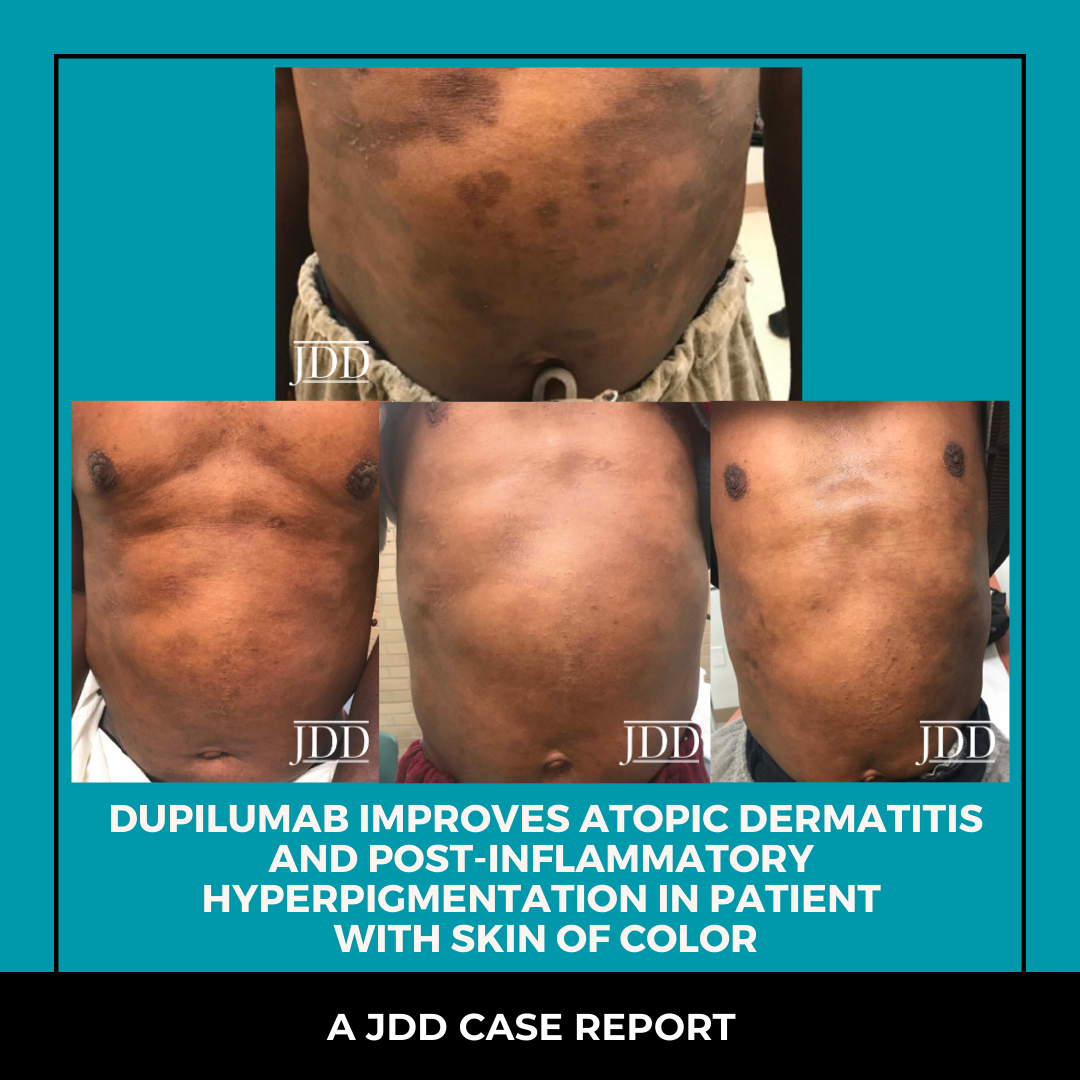
Atopic dermatitis is a chronic inflammatory skin condition that affects up to one fifth of the population in developed countries.1 It is characterized by relapsing pruritic patches and plaques with exudation, crusting, scaling, fissures, and lichenification in later stages.2 Atopic dermatitis lesions may be intensely itchy and elicit discomfort. African Americans are disproportionately affected by atopic dermatitis compared to their Caucasian counterparts, 19.3% and 16.1%, respectively.3 Additionally, atopic dermatitis may be more severe in patients with skin of color and for non-Hispanic black and Hispanic children, is more likely to persist into adulthood.4 Atopic dermatitis in skin of color patients may be particularly distressing due to post-inflammatory hyperpigmentation, which often leads to psychosocial effects and negative impacts on quality of life and productivity.5 In vivo, atopic dermatitis is active in both lesional and non-lesional skin.6 We highlight a case in which treating atopic dermatitis aggressively in a patient of African descent not only leads to clinically improved areas of atopic dermatitis and post-inflammatory hyperpigmentation, but also improves hyperpigmentation in non-lesional skin.
A 53-year-old male of African-descent presented with a 1-year history of worsening pruritic rash. He was applying petroleum jelly without relief. Past medical history was significant for deaf-ness and iron deficiency. On physical exam, there were multiple hyperpigmented plaques, hyperpigmented lichenified plaques, and hyperpigmented patches on the trunk, extremities, buttocks, neck, and face. The patient was diagnosed with moderate-se-vere atopic dermatitis. Triamcinolone ointment 0.1%, tacrolimus 1% and cetirizine 20 mg po daily were prescribed. Gentle skin care and soak and smear technique were reviewed. Two months later, the patient received 600 mg loading dose of dupilumab. Two weeks later, the patient’s atopic dermatitis and pruritus were improved (Figure 1). The patient continued 200 mg sub-cutaneous every 2 weeks resulting in continued improvement of atopic dermatitis, post-inflammatory hyperpigmentation, and apparent hyperpigmentation in non-lesional areas (Figures 2 and 3). Gentle skin care routine emphasized with intermittent use of topical triamcinolone 0.1% ointment or tacrolimus 1% ointment as needed for pruritus. After completion of the fifth month, his next 200 mg injection was performed at the 3-week mark instead of the 2-week mark. His atopic dermatitis flared during this time with pruritus. Dupilumab frequency was re-instated at every 2 weeks. The atopic dermatitis flare resolved, and post-inflammatory hyperpigmentation improved (Figure 4).

FIGURE 1. Improvement of atopic dermatitis two weeks following initiation of dupilumab.

FIGURES 2 AND 3. Continued improvement of atopic dermatitis, post-inflammatory hyperpigmentation and apparent hyperpigmentation in non-lesional areas.

FIGURE 4. Resolution of atopic dermatitis flare and improved post-inflammatory hyperpigmentation.
Atopic dermatitis and post-inflammatory hyperpigmentation are among the top five most common chief complaints seen by dermatologists in skin of color patients. A study conducted on patients that presented to the Skin of Color Center at St. Luke’s-Roosevelt Hospital Center in New York, NY found dyschromias, including post-inflammatory hyperpigmentation, to be the second most common diagnosis in African-American patients, while it was not even among the top ten diagnoses in Caucasian patients.7 Atopic dermatitis often leads to post-inflammatory pigment alteration, most commonly post-inflammatory hyperpigmentation, in those with skin of color.8 Chronic inflammation results in increased melanocyte density, hyperplasia, and hypertrophy.9 This strongly suggests increased function of melanocytes and explains why inflammatory conditions such as atopic dermatitis cause hyperpigmentation. Post-inflammatory hyperpigmentation tends to be more persistent and clinically visible in patients with darker skin tones.10
Dupilumab is a monoclonal antibody that blocks the IL-4 alpha receptor and therefore inhibits IL-4 and IL-13 signaling, preventing the release of type 2 cytokines that promote inflammation in atopic dermatitis.11 A randomized control trial of 54 patients treated with dupilumab resulted in reduced cellular in-filtrates and significant clinical improvement.11 After 16 weeks of treatment, researchers observed reversal of lesional atopic dermatitis phenotype.11
In this case, the post-inflammatory hyperpigmentation was quite severe. After initiation of dupilumab, clinical improvement of the post-inflammatory hyperpigmentation, and lightening of overall skin tone was noted. Suarez et al. compared chronic atopic dermatitis lesional skin, non-lesional skin, and normal skin biopsies and found that non-lesional skin has cutaneous T-cell expansion.6 Non-lesional and lesional skin differ from normal skin in regards to keratinocyte terminal differentiation and inflammatory pathways.6 The abnormalities seen in lesional atopic dermatitis skin are also seen in non-lesional skin, which suggests that the total body surface area of skin in patients with atopic dermatitis is abnormal, even if it appears normal clinically.6 This is especially important in skin of color patients who are more prone to residual effects of atopic dermatitis such as post-inflammatory hyperpigmentation.
Systemically treating moderate-severe atopic dermatitis with dupilumab in skin of color patients with significant, distressing hyperpigmentation should be considered. Reducing hyperpig-mentation in non-clinically apparent areas of atopic dermatitis and evident post-inflammatory hyperpigmentation areas may contribute positively to quality of life. For skin of color patients, aggressive treatment with duplimab may accelerate the return of the patient’s overall normal skin tone.
Post-inflammatory hyperpigmentation often comes with psy-chosocial impairments. A study assessing quality of life found that patients with atopic dermatitis reported significantly more mood and sleep disorders compared to controls.5 These patients had significantly reduced health related quality of life on physical and mental domains.5 In a study of 419 patients, those with post-inflammatory hyperpigmentation had higher scores on the Dermatology Life Quality Index (DLQI) survey, which indicates poorer quality of life, when compared to patients with other disorders of hyperpigmentation.12 Additionally, the study demonstrated that DLQI scores were higher in women and those younger than 35 years of age. Having a graduate level education was associated with significantly lower DLQI scores, showing that patients with lower education level had a more negative impact on quality of life.12 Atopic dermatitis is a systemic disease. Dupilumab’s impact on post-inflammatory hyperpigmentation and apparent hyperpigmentation in non-lesional skin empha-sizes the scientific data of atopic dermatitis activity in lesional and non-lesional skin. When considering whether to treat atop-ic dermatitis aggressively, it is essential to consider the overall impact of the disease including the psychosocial burden, subse-quent post-inflammatory hyperpigmentation and in some cases overall skin hyperpigmentation. Patients with atopic dermatitis experience higher rates of anxiety, depression, sleep disorders, and decreased work productivity.5 Additionally, the resulting post-inflammatory hyperpigmentation can negatively impact quality of life. The burden of atopic dermatitis in patients with skin of color goes way beyond pruritus. In our case, aggressive treatment with dupilumab resulted in improvement of the ap-parent hyperpigmentation in clinically non-lesional skin (but likely scientifically lesional skin), post-inflammatory hyperpigmentation and atopic dermatitis.
There are no potential perceived conflicts of interest and/or sup-port, financial interests, or patents for Ciara Grayson.
Dr. Heath is a consultant for Sanofi-Regeneron and Pfizer.
Originally published in the Journal of Drugs in Dermatology in July 2020.
Grayson, C., & Heath, C. R. (2020). Dupilumab Improves Atopic Dermatitis and Post-Inflammatory Hyperpigmentation in Patient With Skin of Color. Journal of drugs in dermatology: JDD, 19(7), 776-778.
https://jddonline.com/articles/dermatology/S1545961620P0776X
Content and images republished with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
The Journal of Drugs in Dermatology is available complimentary to US dermatologists, US dermatology residents, and US dermatology NP/PA. Create an account on JDDonline.com and access over 15 years of PubMed/MEDLINE archived content.
Did you enjoy this case report? You can find more here.

The ODAC Dermatology, Aesthetic & Surgical Conference (ODAC) recently announced changes to its advisory committee. Dermatologist Adam Friedman, MD, will now serve as ODAC co-chair. Dermatologist and Mohs surgeon James Spencer, MD, will now serve as ODAC co-chair emeritus.
Dr. Friedman, who has served as ODAC medical director since 2017, will now oversee ODAC’s medical dermatology offerings. He will serve alongside dermatologists and Mohs surgeons Joel Cohen, MD, who is co-chair of procedural dermatology, and Susan Weinkle, MD, who is co-chair of aesthetic dermatology. Dr. Friedman also is chair of the GW SMHS Department of Dermatology in Washington, D.C., and is the founding director of the GW Dermatology Residency Program, director of Translational Research in the Department of Dermatology and director of the Supportive Oncodermatology Program at the GW Cancer Center.
“Dr. Friedman has a wealth of knowledge on both medical dermatology and medical education, including how to create compelling educational experiences that translate into improved patient care,” said Shelley Tanner, CEO and president of SanovaWorks, which produces ODAC. “We look forward to his continued contributions for years to come.”
Dr. Spencer, who has served as ODAC chair for 10 years, will now serve as a senior advisor. He will also continue lecturing at ODAC on skin cancer related topics. Dr. Spencer is in private practice in St. Petersburg, Fla., and also serves as clinical professor of dermatology at The Mount Sinai School of Medicine in New York.
“Dr. Spencer has been instrumental in ODAC’s growth since the conference’s inception,” said Ms. Tanner. “We are grateful for his leadership and look forward to his continued impact through his advisory role.”
ODAC, which was founded in 2003, historically attracts nearly 800 dermatology physicians and allied health professionals each year. The 2022 event will take place January 14-17 at the Rosen Shingle Creek in Orlando.

New York (Mar. 17, 2021) – Adam Friedman, MD, medical director of the ODAC Dermatology, Aesthetic & Surgical Conference (ODAC) was recently named chair of the GW SMHS Department of Dermatology in Washington, D.C. Dr. Friedman has served as interim chair since February 2019, and is the founding director of the GW Dermatology Residency Program, director of Translational Research in the Department of Dermatology and director of the Supportive Oncodermatology Program at the GW Cancer Center.
During his time as interim chair, Dr. Friedman further strengthened collaborative ties between ODAC and GW SMHS through multiple and ongoing educational activities, including the GW Translational Science Lecture Series, the award-winning Krazy Kodachromes, and more recently, the 2020 DCAD conference, the GW Appraisal of Acne conference and the Core Crusher Basic Boot Camp Exam Prep Course.
“Dr. Friedman has worked tirelessly to ensure all dermatologists have access to the latest educational developments in the specialty,” said Shelley Tanner, CEO and president of SanovaWorks, which produces ODAC. “He expertly knows how to engage audiences in their education, creating programs that make learning compelling and applicable to daily practice. We are thankful to have his insight at work in our programs.”
Dr. Friedman has served as ODAC medical director since 2017. In this role, Dr. Friedman has been instrumental in cultivating and expanding the medical dermatology section of the educational program, in addition to generating opportunities for residents.
Dr. Friedman also serves on the editorial board of the Journal of Drugs in Dermatology (JDD), hosts the JDD Podcast and is the senior editor of and chairs the Derm In-Review Advisory Council. JDD and Derm In-Review are also products of SanovaWorks.
ODAC, which began in 2003, historically attracts nearly 700 dermatology physicians, residents, nurse practitioners and physician assistants each year. The 2022 event will take place January 14-17 at the Rosen Shingle Creek in Orlando.
###
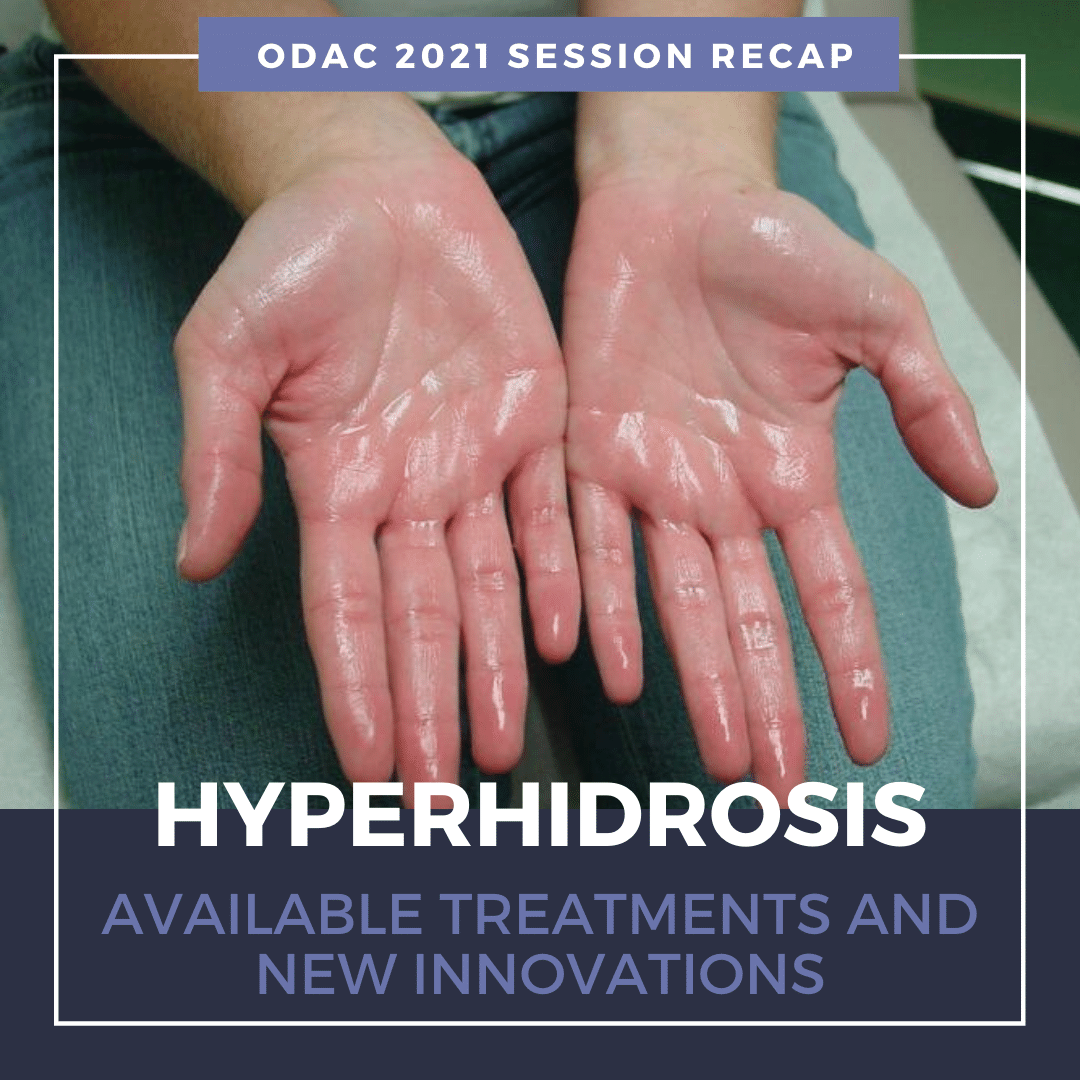
Source: Next Steps in Derm
Primary HH is defined as excessive, bilateral, and generally symmetrical sweating at abnormal levels unprompted by activity or environment.
Hyperhidrosis is characterized by abnormal sweating beyond what is needed for thermoregulation. It is not a normal physiologic response. Nearly 15 million people in the United States suffer from hyperhidrosis and half of those individuals have axillary hyperhidrosis. HH peaks in adulthood and approximately two-thirds of these individuals have never discussed their primary axillary hyperhidrosis with a healthcare professional.
Why aren’t more patients seeking help for their abnormally excessive sweating?
Many of these patients do not realize their excessive sweating is a medical condition and are unaware of protentional treatment options. On average, patients wait at least 10 years before seeking medical help for their abnormally excessive sweating1.
Patients with hyperhidrosis are reluctant to seek medical care, despite the negative impact on their quality of life.
Primary Focal Hyperhidrosis is defined as excessive focal sweating of at least 6 months duration without any obvious cause with at least two of the following features:
90% of all diagnosed cases of HH are primary and two-thirds of all HH patients report a positive family history.
Secondary Generalized Hyperhidrosis can be caused by or associated with another medical condition or results as a side effect of a medication. It usually presents with large areas of the body affected. Patients with secondary HH may experience sweating even when they are sleeping. It is important to differentiate between primary and secondary hyperhidrosis. Review the patient’s medical history and review of systems should point to any secondary causes. Patients who do not fit the classic pattern of primary hyperhidrosis should undergo further evaluation, and may need laboratory studies or radiographic evaluation.
There is no evidence that Covid-19 can be transmitted through sweat. The virus is transmitted by respiratory droplets. Dr. Adam Friedman notes that sweat could actually help prevent the transmission of Covid-19 due to the inherent antimicrobial activity of sweat. For anyone worried about transmission of the virus, it’s important to emphasize key tenets voiced from experts:
For more information, visit the International Hyperhidrosis Society’s (IHS) website: www.sweathelp.org
IHS is the only independent, non-profit, global organization that strives to improve quality of life among those affected by hyperhidrosis.
A wide range of techniques has been utilized in the treatment of HH. First-line therapy for HH is topical formulations. Over-the-counter antiperspirants are usually not strong enough to significantly improve excessive sweating. Prescription aluminum salts are usually the first-line treatment for HH. The aluminum salts act as a plug, precipitating and blocking the sweat ducts. Sweating is reduced in the evening. Thus, application to dry body surfaces at night is ideal. Non-medicated deodorant can be applied in the morning after bathing. The fragrance from deodorants can be used to mask body odor from the microbiome of the skin.
Topical Aluminum Pearls:
Topical antiperspirants are just not that effective for hyperhidrosis.
While over-the-counter products are most commonly recommended, they offer the least patient satisfaction. Topical antiperspirants are safe and simple to use. However, application is time-consuming, only provides temporary relief, and may cause skin irritation at the application site.
Fortunately, there are novel topical therapies available to patients with excessive underarm sweating, or axillary hyperhidrosis. Topical glycopyrronium tosylate (GT) wipes are FDA approved for treatment of axillary HH. This is the first and only prescription cloth towelette approved to treat excessive underarm sweating. GT works by blocking receptors responsible for sweat gland activation1. A significant number of patients can see improvement as early as 1 week. After 4 weeks of treatment in the clinical trials, GT resulted in substantially greater improvements compared to the control group. Patients were happy with the fast onset of effect and reported overall improved quality of life2:
Dr. Friedman notes that use of topical GT for treatment of palmar/plantar hyperhidrosis is off-label. He instructs his patients to rub the towelette between hands until dry, apply Aquaphor, and then wear gloves for at least 1 hour, in order to achieve clinical benefits.
It is important to monitor for anticholinergic side effects. The most common reported adverse effects include dry mouth and mydriasis. Use of gloves with the towelette and careful handwashing can help mitigate anticholinergic side effects. GT is non-invasive, effective, and well-tolerated. There is minimal irritation and can be safely used in pediatric populations. Aside from long-term therapy and potential for cost issues, topical GT provides clinically meaningful benefits for patients with primary axillary hyperhidrosis.
Iontophoresis is a process of transdermal drug delivery by use of a voltage gradient on the skin. It is often recommended for patients who have failed topical therapies or in patients with HH of the palms and soles. During iontophoresis, a medical device is used to pass a mild electrical current through water and through the skin’s surface1. Aluminum chloride or anticholinergics can be added to the water to help draw electric current. This non-surgical method is painless and effective. However, it requires long-term, weekly therapy to maintain efficacy. Of note, iontophoresis is contraindicated in patients with pacemakers or implants, or during pregnancy.
Non-invasive microwave technology uses thermal energy to ablate sweat glands. The device is FDA approved for treatment of severe axillary HH. The treatment is performed in a physician’s office with local anesthesia. Patients typically require 1-3 treatments to achieve long-lasting results. There is little to no discomfort during the procedure. Side effects are minor and include underarm swelling, redness, and tenderness lasting for several days. Numbness and tingling can occur in the upper arm or armpit and may last for about 5 weeks1.
There are no systemic agents FDA approved for treatment of HH. Most data for systemic treatment comes from case reports or small case series. Systemic treatment may be more helpful in multifocal hyperhidrosis or hyperhidrosis of spinal cord injury. The two most common prescribed oral agents include Glycopyrrolate and Oxybutynin.
Glycopyrrolate does not cross the blood-brain barrier, resulting in less CNS effects. There is also an oral solution available for pediatric populations. Oxybutynin is safe in children as well. These therapies are cost-effective, but long-term therapy is required.
There is a risk of hyperthermia in pediatric patients taking systemic anticholinergics. It is important to watch for behavioral changes, as well as drowsiness, dizziness and confusion. Despite the efficacy, most patients discontinue therapy due to anticholinergic side effects.
Other systemic therapies include beta-blockers and Clonidine. Beta-blockers can be used for social phobias/performance anxiety. However, it is contraindicated in patients with bradycardia, AV block, or asthma. Of note, beta-blockers are a common cause of drug-induced psoriasis or exacerbation of psoriasis. Consider other treatment options in patients suffering from both psoriasis and HH. Clonidine has been evaluated in small case series. It is a great medication in treating patients with both hyperhidrosis and flushing.
OnabotulinumtoxinA is FDA approved for axillary hyperhidrosis unresponsive to other therapies. It prevents release of acetylcholine from the neuromuscular junction. Injection technique involves a grid pattern (mapped via surgical marker) using a 30-gauge needle. Injection depth is approximately 2 mm and at a 45º angle to the skin surface with bevel side up. Injections are spaced 1-2cm apart for a total of 50 units injected per axilla.
The 2021 ODAC Dermatology, Aesthetic & Surgical Conference took place virtually January 14 – 17, 2021. Below is a current conference coverage recap. Additional articles will be added and available soon.
Source: MDEdge Dermatology
Source: MDEdge Dermatology
Source: DermatologyTimes
Source: DermatologyTimes
Click here to view the full poster PDF.
The following poster was presented at the 2021 Virtual ODAC Dermatology, Aesthetic & Surgical Conference.
Authors: Morgan Arnold MD, Elise Weisert BS, Paige Hoyer MD, Janice Wilson MD, Brandon Goodwin MD
Cutaneous collagenous vasculopathy (CCV) is a rare acquired idiopathic microangiopathy that affects the superficial cutaneous vessels. We describe the use of intense pulsed light (IPL) treatment in a case of CCV resulting in clinical and dermoscopic improvement. A 73-year-old Caucasian female presented with a rash on the arms and legs spreading proximally. Histopathology revealed abundant superficial dilated telangiectasia with concentric perivascular hyalinized collagen deposition and hyalinized material stained positively for Periodic-acid Schiff-Diastase resistant, confirming a diagnosis of CCV. Intense Pulsed Light (IPL) and Nd:YAG (neodymium-doped yttrium aluminum garnet) test spots were performed, with marked improvement with IPL therapy on follow-up. Two subsequent full IPL treatments were performed on patient’s bilateral arms, exhibiting significant clinical and dermoscopic improvement. Though effective treatments for IPL are scarce in the literature, there are reports of treatment with Multiplex PDL 595-nm/Nd:YAG 1,064-nm laser and optimized pulsed light. Furthermore, comparable entities to CCV such as generalized essential telangiectasia and poikiloderma have also been shown to be successfully treated with IPL. We present the use of IPL for successful cosmetic therapy in a patient with CCV.

For most dermatologic conditions, my mantra for treatment tends to be “less is more”. I prefer to use the fewest number of creams, pills, and steps to achieve the best results. However, after watching this year’s ODAC Sneak Peek Inflammatory Diseases Symposium, I may have a new mantra for treating my rosacea patients – “forks, spoons, and knives”.
At the ODAC 2021 Pre-Conference Sneak Peek Inflammatory Diseases Symposium, Dr. Julie Harper, dermatologist at the Dermatology and Skin Care Center of Birmingham and Founding Director of the American Acne and Rosacea Society, built a case for use of combination therapy for rosacea. It is well known that there are four subtypes of rosacea – erythematotelangiectatic, papulopustular, phymatous, and ocular. However, most patients don’t fall into one subtype, but rather, many experience subtype overlap. This is why Dr. Harper believes that clinicians should “start subtyping lesions” and treat all the lesions that are observed, even if that means use of multiple therapeutic agents.
Not only are there multiple targets clinically, but treatment for rosacea can also be targeted on a cellular level. The role of innate immunity including cathelicidins, specifically LL-37, and toll-like receptor 2 induction via demodex has been described in the pathogenesis of rosacea. But did you know that many of the well-known triggers of rosacea such as heat, stress, exercise, and spice have been implicated to affect rosacea on a cellular level? I certainly didn’t! Dr. Harper explained that common triggers of rosacea cause neurogenic inflammation via induction transient receptor potential channels to release substance P and calcitonin gene-related peptide, which cause vasodilation.
To better understand therapeutic options, Dr. Harper compares the various treatments to utensils, categorizing them into forks, spoons, or knives. She states that treating rosacea is like eating a meal – you can’t get by with just one utensil. While a spork would be a plausible loophole to this one-utensil-meal challenge, we don’t quite have a spork for treating rosacea (yet!). So what exactly are the utensils that Dr. Harper explained?
Forks are medications that treat papules and pustules, including:
Spoons should be utilized for persistent background erythema, such as:
Finally, knives are device-based treatments:
Before showing us the evidence that combination therapy works, Dr. Harper described the goals of combination therapy:
First, she reviewed a JDD article (Fowler J. J Drugs Dermatol. 2007;6(6)641-646) that combined two forks: modified release doxycycline and metronidazole gel. This 16-week study compared combination modified-release doxycycline with metronidazole 1% gel to metronidazole 1% gel with placebo. Metronidazole was discontinued at week 12 and doxycycline or placebo continued through week 16. At week 4, patients who received combination therapy had greater reduction of inflammatory lesion counts and were generally better faster. Then after week 12, those who continued on modified release doxycycline had better sustained results.
Next, Dr. Harper reviewed another JDD study (Stein Gold L, Papp K, et al. J Drugs Dermatol. 2017;16(9):909-916) that combined a fork and a spoon – ivermectin and brimonidine – to treat both moderate to severe erythematotelangiectatic and papulopustular rosacea. Three groups were identified in this study – one receiving vehicle only, one receiving ivermectin for 12 weeks with addition of bromonidine at week 4, and one receiving both ivermectin and brimonidine for 12 weeks. The most striking result from this study was that those who used combination therapy for 12 weeks had double the rate of improvement of redness in the three hours after brimonidine use. Dr. Harper explained that despite the use of a really good fork (ivermectin), there was still enough residual redness that the spoon (brimonidine) could make a meaningful impact. Thus, targeting inflammation and pustules alone will not lessen background erythema.

This year, due to the global pandemic, we are hosting ODAC Dermatology, Aesthetic and Surgical conference, virtually. ODAC is committed to providing high-quality education in an engaging virtual format with top speakers and important topics.
With nearly 1,000 US attendees registered, ODAC will provide a unique virtual experience that will continue to drive dermatology education and networking forward.
We appreciate all the effort that it takes to change direction and to make such an important and impactful event happen. We are deeply grateful to our sponsors, faculty and attendees.
Please take a moment to acknowledge and thank our gracious supporters by visiting their sponsor page in ODAC Virtual app.
Please see the resources below to discover our data and explore our resources in our sponsor page.

Cassiopea, Inc. is a specialty pharmaceutical company developing and commercializing prescription drugs with novel mechanisms of action to address long-standing and essential dermatological conditions such as acne, androgenetic alopecia and genital warts. Learn more about our company at www.cassiopea.com.
Our commitment to dermatology is built around a senior leadership team with deep roots and experience in the specialty. The management team is focused on providing unique treatment options, and to drive continued research and development in Dermatology, moving us to the forefront of the U.S. market.
We are excited to support dermatology healthcare professionals by contributing to the ODAC 2021 Conference.
Galderma, the world’s largest independent global dermatology company, was created in 1981 and is now present in over 100 countries with an extensive product portfolio of prescription medicines, aesthetics solutions and consumer care products. The company partners with health care practitioners around the world to meet the skin health needs of people throughout their lifetime. Galderma is a leader in research and development of scientifically-defined and medically-proven solutions for the skin. For more information, please visit www.galderma.com/us.
Incyte is a global biopharmaceutical company that is focused on finding solutions for serious unmet medical needs through the discovery, development and commercialization of novel medicines.
Since 2002, Incyte has remained committed to the relentless pursuit of science that can improve the lives of patients, make a difference in healthcare and build sustainable value for our stakeholders. The Company is advancing a diversified portfolio of clinical candidates across Oncology and Inflammation & Autoimmunity. Our research and development efforts in Dermatology are focused on a number of immune-mediated dermatologic conditions with a high unmet medical need, including atopic dermatitis, vitiligo, and hidradenitis suppurativa.
Headquartered in Wilmington, Delaware, Incyte has operations in North America, Europe and Asia.
For more information, visit Incyte.com and follow @Incyte.
Visit the Incyte Dermatology Virtual Booth.
At Aveeno®, groundbreaking science transforms nature’s ingredients into clinically proven products that help soothe, strengthen, and restore the moisture barrier. Our oat, soy, and feverfew ingredients—derived from nature and uniquely formulated to optimize skin health and beauty—are supported by 75 years of published data, demonstrating the scientific rigor behind every result. Visit AveenoMD.com to learn about our new products, plus access clinical resources, patient resources, and product samples.
The #1 dermatologist recommended skincare brand continually elevates the science of skincare, delivering new products and innovations that support your treatment guidance. Visit NeutrogenaMD.com to learn what’s new, plus access clinical resources, patient resources, and product samples. NeutrogenaMD.com – dedicated to dermatology professionals.
Our brands are dedicated to dermatology with offerings in professional skincare and cosmetics. Each brand is created by dermatologists or works in partnership with dermatologists to meet the health and safety standards for patients. Please visit the L’Oréal booth.
Novartis is a leading global medicines company, using innovative science and digital technologies to create treatments in areas of great medical need. In our quest to find new medicines, we consistently rank among the world’s top companies investing in research and development. Novartis products reach more than 800 million people globally and we are finding innovative ways to expand access to our latest treatments. About 109,000 people of more than 145 nationalities work at Novartis around the world. Find out more at www.novartis.com.
We hope you will take a moment to visit the COSENTYX® (secukinumab) Virtual Booth Experience to learn more about the Complete Cosentyx Approach.

Ortho Dermatologics is a specialty pharmaceutical business with the number one prescribed acne franchise and a portfolio of dermatology treatments in additional therapeutic areas including atopic dermatitis, fungal infections and psoriasis. Led by a team with deep experience in dermatology, we are dedicated to building meaningful connections with healthcare providers and their patients. Our ongoing commitment to the dermatology community shows through our pipeline of novel compounds and focused philanthropic activity here and around the globe.
Regeneron is a leading biotechnology company that invents medicines for people with serious diseases. Founded and led for over 30 years by physician-scientists, our unique ability to repeatedly and consistently translate science into medicine has led to seven FDA-approved treatments and numerous product candidates in development, all of which were homegrown in our laboratories.
Sanofi is dedicated to supporting people through their health challenges. We are a global biopharmaceutical company focused on human health. We stand by the few who suffer from rare diseases and the millions with long-term chronic conditions. With more than 100,000 people in 100 countries, Sanofi is transforming scientific innovation around the globe.
Please click the link below to visit our virtual booth!
https://www.dupixenthcp.com/virtualcongress
At UCB, we come together every day to work, laser-focused, on a simple question: How will this create value for people living with severe diseases? Patient value is not just what we say, but how we how we live. It is our culture of care, embodied by our patient value strategy. That’s because how we do business – from discovery to development to delivery – has been transformed and redesigned around the patient and their individual experience. Patients are at the heart of everything we do, inspiring us, driving our scientific discovery, and leading us to rethink the patient experience. By fulfilling our commitment, driving innovation, and providing patients a meaningful experience, more impactful solutions are on the horizon.
With a team of approximately 7,500 employees and operations in nearly 40 countries, we are a global biopharmaceutical company investing more than a quarter of our revenue in cutting-edge scientific research to meet unmet patient needs. Global headquarters are in Brussels, Belgium, with U.S. headquarters in Atlanta, Georgia. Additional U.S. UCB sites include global clinical development in Raleigh, North Carolina, research supporting UCB’s pipeline in Boston, Massachusetts (Bedford and Cambridge), Seattle, Washington, and Durham, North Carolina as part of our acquisition of Element Genomics, as well as an office in Washington, D.C.
CLICK to ENTER Virtual Experience
Learn what integrated skin care is and how to incorporate skincare to compliment your in-office procedures. All US-based practitioners that attend the full webinar, will receive a 30 mL CE Ferulic!
Date: Tuesday, December 8, 2020
Time: 7:00 – 8:00 PM ET
Faculty: Sheila Barbarino, MD, FACS, FAAO, FAACS
The American Academy of Dermatology (AAD) 2021 has announced the cancelation of the annual meeting in March.
On November 23, 2020, a message was sent to all Academy members and all attendees registered for the 2021 Annual Meeting schedule for March 19 – 23, 2021 in San Francisco, California.
Like ODAC Dermatology Aesthetic and Surgical conference, the health and safety of attendees, faculty, and sponsors comes first. Given the current situation with the pandemic, ODAC is committed to providing high-quality education in an engaging virtual format with top speakers and important topics.
Although we will miss seeing everyone in person at ODAC and the AAD 2021, we aim to provide a unique virtual experience that will continue to drive dermatology education and networking forward.
Experience ODAC virtually thought the free sneak peek Dec, 3rd, Resident Week Jan 8th and the full conference ODAC Jan. 14th. ODAC offers a unique 100% live experience. ODAC is not pre-recorded, offering hours of panels, CME, live polling and an enhanced attendee experience.

When we think about skin, a few things come to mind: protection, temperature regulation, sensation. However, there is growing interest in the microbiome of the skin. Our skin flora can be likened to an invisible ecosystem. Similar to fingerprints, it is unique to each individual. The complexity of the skin microbiome is continuing to be researched. This research is paving the way to improve our understanding of the relationship between acne and dysbiosis.
At the GW Virtual Appraisal of Advances in Acne Conference, Dr. Adam Friedman discussed Microbiome Manipulation in the Management of Acne. His lecture provided insight on the microenvironment of the skin and how the diversity in skin flora can affect disease processes such as acne.
First, let me share a few pearls from Dr. Friedman’s lecture.
The skin is a physical barrier against invasion by pathogenic organisms and foreign substances. The skin is also an ecosystem, host to a variety of microorganisms that are typically harmless.
The habitat of the skin varies topographically and there are several factors that contribute to this unique variation among individuals.
The cutaneous immune system modulates and can be modulated by these commensal microorganisms. Dysbiosis, which directly refers to decreased microbial diversity, is directly linked to dysregulation of the skin immune response is evident in several skin disorders.
When we think about the skin barrier, we usually think about the hydrophilic corneocytes and hydrophobic lipids that make up this security guard for your skin. However, we do not necessarily think about the invisible barrier that protects the skin, which is composed of numerous microorganisms. Both of these components are vital to the structural stability of the skin barrier. If this invisible barrier is disrupted, this may lead to skin disease. Why are these commensal organisms so important?
Role of commensal organisms on the skin:
We all have a unique skin microbiome. What contributes to the variability of the skin microbiome?
Factors contributing to individual variations in skin microflora:
Read more….
Hosted by George Washington University, in Partnership with ODAC Dermatology, Aesthetic & Surgical Conference and Next Steps in Derm
Even during a global pandemic we cannot forget that Acne Vulgaris is one of if not THE most common skin condition afflicting our patients and the general populace. With the disruption of clinics and conferences, innovative vehicles for the dissemination of the most up to date data and expert anecdote are certainly and sorely needed.
Enter the GW Virtual Acne Appraisal Conference: A 3 hour program that promises to pander to your pimple popping practices with short but sweet lectures from the acne gurus covering the gamut of the big A. From treatments to treats, from considering the microbiome to unique treatment approaches in specific patient populations, we will cover it all. And if that wasn’t enough, we will round it out with a perusal of the therapeutic pipeline. It will be all that and a bag of chips (which may or may not cause acne…you need to tune in to find out).
8:00 – 8:15 – Introduction and Welcome
8:15 – Topical Management of Acne– James Q. Del Rosso, DO, FAOCD, FAAD
8:30 – Use of Hormonal Therapies in Acne– Julie Harper, MD
8:50 – Use of Antibiotics in Acne – Neal Bhatia, MD
9:10 – Issues with Isotretinoin: Fact vs. Fiction – Jenna C. Lester, MD
9:30 – Microbiome Manipulation for the Management of Acne – Adam Friedman, MD, FAAD
9:45 – Diet and Alternative Therapies: What to know for Acne management – Vivian Shi, MD
10:00 – Management Considerations for Skin of Color Patients with Acne –Andrew Alexis, MD, MPH
10:20 – Managing Acne in the LGBTQ+ Population – Angelo Landriscina, MD
10:40 – New and Emerging Therapies for Acne – Leon Kircik, MD
This webinar was previously recorded on July 1, 2020 and is now available on demand.
Business intellect, a vital aspect of managing a practice, is not taught in residency. From the infancy of their training, dermatologists are trained to think broadly and scrupulously, using each clue, each corporeal sense, and each available tool to accurately diagnose and manage a plethora of cutaneous conditions. After residency, dermatologists set out armed with the knowledge and drive to deliver expert care to their future patients. However, despite their education and best intentions, lack of business acumen can hinder even the brightest and most motivated of practitioners. In order to enlighten oneself in the complicated field of business management, clinicians are left to fend for themselves, often learning as they go, sometimes making unnecessary mistakes, and adjusting their business practices reactively. Retrospective “trial and error” learning is time-consuming, cumbersome, and costly. Why not short track and get the goods without the trial and error, making costly mistakes and taking years. The new book, The Business of Dermatology is a cornerstone achievement in the standardization of business education for dermatologists.
Edited by Drs. Jeffrey S. Dover and Kavita Mariwalla, and authored by impressive experts in the field, The Business of Dermatology offers a comprehensive guide to opening, maintaining, and sustaining a practice. To start, the power of this textbook fundamentally lies in the experience and scope of its authorship. The authors were hand-selected by the editors ensuring that each chapter was written by a tried and true expert in that subject. Unlike other textbooks in the field of business management and administration that are primarily written by individuals from the business world, some of whom have no insight into the inner machinations of the medical world, or hands-on experience, the authors of this book are well-known, respected dermatologists that hail from thriving practices of their own. The reader has an unprecedented opportunity to learn from the firsthand experiences of top authorities who live and breathe dermatology. Using conversational prose, the authors depict their experiences, trials, and errors, employing specific real-world examples and scenarios while tackling each subject.
A notable forte of The Business of Dermatology is the sheer breadth and range of topics discussed in the textbook by medical as well as surgical dermatologists. Opening and managing a practice is a daunting endeavor with twists, turns, and hidden hurdles that one cannot foresee until stumbling across them. The Business of Dermatology unveils those twists, turns, and hurdles for the reader, taking the “guessing game” out of the equation. Fifty-five chapters elucidate every aspect of running a practice, covering all practice-relevant topics, including office space and equipment, managing financials, diverse practice models, human resources, employment considerations, patient issues, pricing, essential surgical tools/supplies, marketing, and much more. The Business of Dermatology lays bare every facet of handling a dermatologic practice, so much so that even a well-run, seasoned practice stands to learn new tools and tips to elevate itself to a higher level.
And now more than ever in the “Time of Covid” we are in desperate need of information from The Business of Dermatology. Many of us are inventing the wheel with the significant changes that are occurring in Dermatology, and the practice of our specialty.
The wealth of knowledge endowed in each chapter is written and formatted in such a style that renders each chapter extremely easy to read and comprehend. First, the prose used in the chapters is conversational – as such, the reader is fully immersed in each topic as if he/she were having a face-to-face chat with the authors. Furthermore, references are used only when absolutely necessary. The reader is not bogged down by superfluous references and discussions that may dim the vital discussion points of the chapters. Finally, embedded within each chapter are practical tips that are immediately implementable and a Top Ten list that highlights the key take-home points, making “reading on the run” possible. The novice practice owner need not fear the residency dogma of “trying to drink from a gushing fire hydrant” with this easy-to-read, catchy and focused textbook.
ODAC Dermatology, Aesthetic & Surgical Conference’s Medical Director, Dr. Adam Friedman, discusses the ODAC 2021 program, reasons to attend and more!
To view the full agenda, click here: https://orlandoderm.org/agenda/
NEW YORK, (June 3, 2020) – Shelley Tanner, SanovaWorks (parent company of ODAC) CEO/President
The below was sent to the employees of SanovaWorks.
This is an issue we should all be aware of, we should all be engaged in, and we should all be actively fighting together against for a solution. Each company, as a collective of humans, has a responsibility to do everything we can to protect our fellow humans and ensure that we all have access to the things we hold dear. We cannot stand by knowing that our fellow Americans are being targeted unjustly from all angles.
On the heels of the global and national devastation of the coronavirus pandemic, we are witness to the glaring evidence of an epidemic that has existed for hundreds of years in the USA, and that is the systematic racism and injustice against black Americans. The devastation that results from this affects lives in literally every facet: education, careers, health, families, finances, safety, etc.
The pandemic unveiled in clear numbers the disparity between black and white communities in this country, where only 13% of the population are African American, yet represent 23% of the deaths. In some states, like Georgia, African Americans make up little more than 30% of the population, yet almost 50% of deaths are from within this group.
On May 25th this year George Floyd, a black man from Minneapolis who is also a brother, a cousin, a nephew, a friend, a boyfriend, a son, and a fellow human, was murdered in a horrific incident that has reinvigorated people to stand up and say that this is not acceptable, spurring the nationwide protests that are not only just, but also necessary to demand change for a reality that has been accepted through complacency and inaction.
For our employees who are impacted by this, we need to support you. As a team and your friends we are here to back you up.
If you don’t already know how you can personally help, I hope you will take the time to learn what we can all be doing at this time to be a part of the solution. You might feel helpless or overwhelmed by this matter, and feel like there is nothing you can do, but this is part of the problem. Doing nothing is a choice and an action. The support we show for one another matters. One of my friends sent me this article on the weekend, for which I was extremely grateful, as it outlines many things we can all be doing for racial justice.
READ What White People Can do for Racial Justice
On June 1, President Obama published an article on how he believes we can use what is happening now as a turning point for real change that is definitely worth the read. In this article there is a link to a very detailed report and toolkit developed while he was in office by the Leadership Conference on Civil and Human Rights, along with a dedicated site of resources and organizations to learn about and get involved with.
READ How to Make this Moment The Turning Point for Real Change
Below is a list of grassroots organizations supporting this cause. I have personally donated, and I encourage you all to consider doing the same. There are many more that I have read about and perhaps that speak to you more personally. I encourage you to look up some of these groups and read about what they are doing.
https://minnesotafreedomfund.org/
https://www.blackvisionsmn.org/
https://www.reclaimtheblock.org/home
https://www.northstarhealthcollective.org/
We as a company will take a moment of silence at 1:30pm ET to reflect on these injustices, and how we personally might help. I would like us all to pause together and show solidarity. For those who choose to sit on their own, know we are with you.
I am committed to ensuring that this is not the end of the conversation for SanovaWorks. Stay tuned for more information and please get in touch with me directly if you have thoughts on this. I welcome all ideas and feedback.
And finally. To ALL of our friends of color: know that we see you, we appreciate you, and we will do everything we can to support you.
Shelley N. Tanner
President/CEO
ODAC Dermatology Conference, in partnership with Next Steps in Derm, interviewed Dr. David Miller, Instructor in Dermatology and Medicine at Harvard Medical School and member of the Department of Dermatology and the Department of Medicine at Massachusetts General Hospital, where he is co-director of the Merkel cell carcinoma treatment program. Watch as he shares important updates on Immuno-Oncology (IO) strategies for melanoma.





Next Steps in Derm, in partnership with ODAC Dermatology, Aesthetic and Surgical Conference, interviewed Dr. Vic Ross, Director of the Scripps Clinic Laser and Cosmetic Dermatology Center in San Diego, CA, on his approach and the various interventions he uses for the treatment of Melasma. Watch as he shares fresh practical pearls immediately useful in your practice.
According to ODAC Vice-Chair Dr. Joel Cohen, Director of AboutSkin Dermatology (Greenwood Village and Lone Tree, Colorado), and Associate Clinical Professor at the University of California at Irvine, the pendulum is swinging back to heavy resurfacing in areas such as around the mouth and around the eyes that really need it. He uses full-field erbium resurfacing and shares why this is the way to go.
Next Steps in Derm, in partnership with ODAC Dermatology, Aesthetic and Surgical Conference interviewed Drs. Susan Weinkle and Jackie Yee to get their expert opinion on how to train the aesthetic eye. Watch as they share their views from a dermatologist and a plastic surgeon perspective.
So many diseases, so few FDA approved indications. Between the mind-numbing time and cost from bench to bottle, it is no surprise that dermatologists, as masters of the integument are the off-label bandits, marrying their wealth of knowledge on the pathophysiology of skin diseases to the mechanisms by which medications work to create an evidenced-based armament of therapies for both common and rare diseases alike. Where a primary care physician sees a blood pressure medication, a dermatologist sees an effective medication for acne. A medication for malaria you say? They use it for a plethora of complex diseases ranging from Lupus to scarring hair loss. The lengthy list of medications used off-label in dermatology continues to grow and for good reason and fortune.
Next Steps in Derm, in partnership with ODAC Dermatology, Aesthetic and Surgical Conference interviewed Dr. Adam Friedman, Professor, Interim Chair of Dermatology, and Residency Program Director at George Washington University, who shared off-label uses of drugs such as Hydroxychloroquine (currently under investigation for the treatment of patients with COVID-19), Pentoxifylline, and Colchicine. A wealth of clinical pearls you don’t want to miss!
Additional video pearls can be found here.
On April, 1, 2020, the Journal of Drugs in Dermatology (JDD) and SanovaWorks brands, including ODAC launched Part I of the webinar series: COVID-19: Urgent Dermatology and Aesthetic Issues for Dermatology.
Over the course of the 2 hours, Joel L. Cohen, MD and 6 different thought leaders joined the COVID-19 conversation, discussing the pressing questions that are on the minds of many dermatologists and providers in the country. The initial broadcast attracted 1,900 registrants and nearly 800 attendees comprised of physicians, residents, fellows, nurse practitioners and physician assistants. Attendees were interested and engaged throughout the entire 2 hours with a 76% average attentiveness and 72% average interest rating.
The on-demand broadcast has attracted over 500 registrants as of April 9th and is available on JDDonline.com.
On April 7, 2020, Part II of the webinar series was broadcasted: COVID-19: Your Questions Answered. Dermatology experts and thought leaders examined the legal and financial concerns of dermatology providers during the global coronavirus pandemic. Experts discussed furlough vs. layoffs; mortgage and rent relief programs; the CARES Act; the pros and cons of leveraging NPs or PAs for teledermatology and more. Then, hear questions answered by our panel of experts; discussed practical tips you can use in your practice right now; and how to move forward with patient care. Part II attracted 1,300 registrants with nearly 700 attendees. Attendees were engaged and interested throughout with an 82% attentiveness average and 75+% interest rating.
The on-demand broadcast of Part II will be available on April 11, 2020 on JDDonline.com.

Source: Journal of Drugs in Dermatology
While the world lives under the shadow of the novel coronavirus (COVID-19) pandemic, dermatologists wonder if the current situation calls for a temporary change in the management of skin conditions.
Immunosuppressive drugs are used ubiquitously in the modern treatment of inflammatory and autoimmune skin diseases like psoriasis, bullous diseases, connective tissue diseases, and many others. Treatment of these conditions is based on the suppression of the patient’s immune system using steroids, steroid-sparing drugs, and biological agents.1
While the effects of the novel coronavirus on the body and its immune system are still being studied, there is overwhelming evidence that the virus could directly or indirectly affect the immune system. In one study, lymphocytopenia was reported in 83.2% of the admitted patients and might be associated with a worse prognosis.2In another study, a steady decline in the lymphocyte counts was recorded in a group of patients who did not survive the infection.3
While the coexisting comorbid medical conditions (such as diabetes or heart disease) are considered as independent predictors of an adverse outcome of the novel coronavirus infection,4 it could be assumed that the chronic inflammatory and autoimmune skin diseases like psoriasis by themselves might imply an additional risk factor of developing more serious symptoms of the novel virus due to their chronicity and effects on the immune system.5
The use of immunosuppressive to treat these conditions can amplify this effect, and it might leave the patient vulnerable to more serious complications should an infection with the novel coronavirus be established. Hence, it may be wise to restrict temporarily the use of immunosuppressive agents including systemic steroids, steroid-sparing agents, and biologics in dermatology daily practice until more evidence is available about their safety in the current pandemic.6As a relates point, the International Psoriasis Council declared an urgent statement on March 11, 2020 that the physician should be alert to the potentially harmful effects of COVID-19 infection on patients with psoriasis and to immediately discontinue or postpone immunosuppressant medications for psoriasis patients diagnosed with COVID-19 disease.7
Clinical photography is a critical tool for the dermatologist and has rapidly become standard of care in the digital era. While a point-and-click approach to photography is sufficient for some circumstances, there are some simple tricks and techniques that will elevate your photography to a new level of professionalism.
Next Steps in Derm, in partnership with ODAC Dermatology, Aesthetic and Surgical Conference interviewed Dr. Justin Finch, Associate Professor of Dermatology at UConn and Co-Founder of Central Connecticut Dermatology who shared his top 3 pearls for improving clinical photography in your practice.
This webinar was previously recorded on April 1st, 2020 and is now available on demand. Click here to access the on-demand recording.
ODAC and JDD invite you to attend a webinar panel to provide discussion, guidance, and leadership for dermatologists and dermatology practices during the global coronavirus pandemic.
Over the course of the 2 hours, 8 different thought leaders will join the conversation, discussing questions that are on the mind of many dermatologists in the country. Click here to register.
MODERATOR
Joel L. Cohen, MD (Director, About Skin Dermatology & Associate Clinical Professor, University of California at Irvine)
AGENDA
6:00-7:00PM
Neal Bhatia, MD (Vice President-elect of the AAD & Director of Clinical Dermatology, Therapeutics Clinical Research)
Adam Friedman, MD (Professor and Interim Chair of Dermatology, GW School of Medicine & Health Sciences)
William D. Humphries (President, Ortho Dermatologics)
Mark Kaufman, MD (Associate Clinical Professor, Icahn School of Medicine at Mount Sinai)
7:00-8:00PM
Sue Ellen Cox, MD (Founder, Aesthetic Solutions)
Kavita Mariwalla, MD (Founder, Mariwalla Dermatology)
Carrie Strom (Senior Vice President, US Medical Aesthetics at Allergan)

Source: ODAC Dermatology Conference’s Parent Company, SanovaWorks
NEW YORK, (Mar. 26, 2020) – Shelley Tanner, SanovaWorks CEO/President
In the wake of COVID 19, I wrote a article about the Top Immediate Needs of a Remote Employee
Regular communication through video conference calls was at the top of my list. I asked the team what their thoughts were and received a great response from Nick.
Nick Gillespie, Assistant Publisher
Sometimes staff can feel that it’s an imposition, but the quality of meetings for those participating via video is infinitely better than just via phone
People quickly become used to the video interface, to the point where it becomes no different from meeting face to face in the office.
Some links about the benefits of face to face meetings (even remote ones):
https://timemanagementninja.com/2012/10/5-reasons-why-meeting-face-to-face-is-best/
https://sebastiancorp.com/10-reasons-video-conferencing-is-better-than-a-conference-call/

Source: Next Steps in Derm
Each week, Next Steps in Derm will be compiling the top news and updates surrounding COVID-19 to keep you up-to-date and informed.
Learn what information can be shared about individuals who have contracted COVID-19, those suspected of exposure to the 2019 Novel Coronavirus, and those with whom information can be shared.
For any questions you have related to the response to HIPAA compliance during coronavirus crisis call (800) 231-4096.
The JDD CME library is now updated to accommodate a growing demand for online CME resources. We expect this demand to grow in light of the cancellation of some medical meetings due to the global COVID-19 situation. Access the CME library here.
The American Academy of Dermatology strongly recommends that patients should not stop biologic therapy without consulting their physicians. Read their interim recommendations here.
Managing your practice through the COVID-19 outbreak
AMA Physician’s Guide to COVID-19
COVID-19: Frequently asked questions

Source: ODAC Dermatology Conference’s Parent Company, SanovaWorks
NEW YORK, (Mar. 23, 2020) Signe Pihlstrand, Vice President, SanovaWorks
In the wake of COVID-19 and the need for social distancing, many companies are having their staff work from home, and a great portion of them don’t have a routine remote policy or have remote processes set up. SanovaWorks has been successfully 100% remote for over six years now, and we gave ourselves many months of preparing, the better part of a year, before launching our remote work culture. These companies unfortunately don’t have that luxury and need to keep their workforce productive and the wheels rolling with an abrupt start to their remote experience. When I think about the most important things a company can do to lay the right foundation for their remote procedures, the plan for how you will communicate regularly is the first thing that comes to mind.
If your team isn’t used to working remotely, you can’t assume that everyone will be on the same page about how to connect. Setting up defined guidelines for when and how you will communicate is so important.
These ideas may seem obvious, but if not set up to make sure everyone has the same idea about what communication looks like, it can really wreck productivity. If everyone is left to their own devices, you could be fielding phone calls, texts, IMs, video chats, and emails from whatever program someone has on their phone or laptop, at all times of the day, or not at all. Remote working requires its own set of procedures, just like you have at the office.
At SanovaWorks we train everyone on our designated tools and procedures and make it a priority to use video chats whenever possible for the best communication and team member connections!

NEW YORK (Mar. 13, 2020) – A Note from Shelley Tanner, SanovaWorks CEO/President
First and foremost, in light of the rapidly evolving global COVID-19 situation, we hope that you and your family are safe and healthy. We send companywide thoughts and prayers to the individuals, families, and other groups who have been impacted by this situation, and hope that things will improve very soon.
While many things are uncertain surrounding this virus, as an organization, SanovaWorks believes in taking action early. We are dedicated to providing the best care and support we can to all our employees and business partners.
We have the extremely good fortune to be functioning already as a virtual company and because of this we hope to be able to provide support and resources to our entire network who might not have the experience we have. Please check our blog for our tips and recommendations for transitioning to and being successful in a remote work environment:https://sanovaworks.com/2020/03/11/top-immediate-needs-of-remote-employees/
In addition to this, in order to protect our teams and others, until further notice, we have issued a complete restriction on all business-related travel. While the CDC has not placed restrictions on domestic travel, they have recently posted travel warnings on their website: https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-in-the-us.html?mod=article_inline
The CDC also provide general recommendations that we should all be following to prevent the spread of this disease:https://www.cdc.gov/coronavirus/2019-ncov/about/prevention.html
We will be working diligently as teams to connect with many of you so that we can share some very interesting ways to accomplish our results in this new, virtual environment. We have many years of experience transitioning traditional programs to digital programs, and launching successful virtual programs. Because we are already positioned as a remote company that produces virtual programs, we hope that we are able to support your own initiatives and bridge the gap this global situation has caused.
And last but not least, with a shout out to Jim Collins who introduced me to the Stockdale Paradox in his book Good To Great, we all need to look squarely at the facts, but have confidence that together we will prevail, as we balance realism with optimism.
Together.
Shelley and the entire SanovaWorks Team
Source: ODAC Dermatology, Aesthetic & Surgical Conference (ODAC) Discovery in Dermatology Poster Session
At the 17th Annual ODAC Dermatology, Aesthetic, and Surgical Conference (ODAC) held January 17-20 in Orlando, FL, Brandon Kirsch, MD, Janet DuBois, MD, Martin N. Zaiac, MD and Deepak Chadha, MS, MBA, RAC presented scientific research of long term data with a novel therapeutic for topical treatment of primary axillary hyperhidrosis in pediatric subjects.
Discovery in Dermatology
The use of retro-metabolically designed drugs in dermatology is novel and has the potential for providing significant therapeutic benefit to pediatric and adult patients.
Sofpironium bromide is an ester analogue of glycopyrrolate that inhibits muscarinic receptors in sweat glands. It was developed according to the principles of retro-metabolic drug design, in which the goal is to create an active compound that is metabolized in vivo to an inactive moiety in a single, predictable reaction. Retro-metabolically designed drugs are rapidly metabolized in the bloodstream, potentially allowing for optimal therapeutic effect at application sites with minimal systemic side effects.
Introduction
~2.1% of the US population aged <18 years has primary hyperhidrosis (HH); ~65% have axillary HH. Long-term safety/tolerability and efficacy of topical HH treatments have rarely been studied in pediatric patients. Sofpironium bromide is a retro-metabolically designed analog of glycopyrrolate (anticholinergic) in development for topical treatment of primary axillary HH. Absorbed drug is rapidly metabolized, potentially allowing optimal local therapeutic effect with minimal systemic effects..
Procedures
21 of 25 subjects (age 9-16 yrs) with primary axillary HH of ≥6 months duration, completing a previous 1-week safety and pharmacokinetic (PK) study (BBI-4000-CL-105), were enrolled. Objectives were to assess safety/tolerability and PK, and explore efficacy of sofpironium bromide gel, 15% applied to both axillae for 24 weeks.
Results
Mean age (SD) 13.3 (2.29) years. 16 subjects completed this 24-week study. 7 had treatment emergent adverse events (TEAEs); 4 with AEs related to study drug, including expected systemic anticholinergic AEs (blurred vision, dry mouth, dry eyes, mydriasis) and local events (pain, pruritus, rash, erythema). 2 subjects discontinued due to TEAEs, including dry eye, dry mouth, local pruritus, local rash. The majority (52.4%) of subjects did not have any local symptoms/signs, and none observed were severe in nature. PK did not show evidence of drug/major metabolite accumulation, with most subjects having concentrations not quantifiable. The validated patient-reported outcome, Hyperhidrosis Disease Severity Measure-Axillary (HDSM-Ax), showed mean (SD) change from baseline (from previous study) to Week 24 of this study of -1.91 (1.038). A -1.00 change shows clinically meaningful improvement.
Conclusion
In this 24-week study in pediatric subjects sofpironium bromide, 15% was safe/well tolerated. Majority of subjects had no TEAE, and there were no severe or serious AEs. There was no evidence of drug accumulation. There was indication of clinically meaningful improvement in axillary HH.

Source: ODAC Dermatology Conference’s Parent Company, SanovaWorks
NEW YORK (Mar. 11, 2020) – A Note from Shelley Tanner, SanovaWorks CEO/President
SanovaWorks transitioned into a 100% virtual company at the end 2012 at the same time press was reporting market leaders like Yahoo and Best Buy stopped all remote work at their companies. To the outside world, it seemed like we were making a crazy decision, heading in the opposite direction from global brand in terms of office culture and environment. We were convinced of the many benefits, so without hesitation we transitioned from two floors of a small office building on Park Avenue South in Manhattan, to a completely remote workforce.
I realize that due to the Coronavirus outbreak many companies are forced to transition some or all of their teams into remote teams without a solid plan, and so I felt compelled to share some of my thoughts on this matter.
If anyone has specific questions please comment on the Linked In post or direct message me and if I can’t answer, I will ask one of my extremely competent virtual team.
Best to all during these challenging times,
Shelley
During the 2020 ODAC Dermatology, Aesthetic and Surgical Conference, Dr. Amy McMichael, Professor and Chair of Dermatology at the Wake Forest University School of Medicine, sat down with Next Steps in Derm to share important updates regarding treatments on the horizon for the most common forms of hair loss. Dr. McMichael will be presenting at Skin of Color Update 2020 with lectures including Hair & Scalp Disorders in SOC: Diagnostic Approaches and Hot Topics & Controversies in Photoprotection: Making sense of it all.
Source: George Washington University, ODAC and JDD
A new study from the George Washington University found that many dermatologists are unprepared to respond to biological disasters and that the specialty would benefit from formal preparedness training.
WASHINGTON (Jan. 30, 2020) — The dermatology community is inadequately prepared for a biological disaster and would benefit from a formal preparedness training program, according to a study from the George Washington University (GW). The article is published in the Journal of Drugs in Dermatology.
Natural and man-made disasters can cause a range of dermatologic conditions due to environmental exposures, such as secondary infections following a flood, irritation from blistering agents used in chemical warfare, and acute and chronic effects of cutaneous radiation syndrome. A 2003 survey revealed that 88% of dermatologists felt unprepared to respond to a biological attack — this new survey shows that the need for training still exists.
“Recognizing and diagnosing the conditions that can arise following a disaster requires diagnostic acumen, knowledge on reporting, and short- and long-term management strategies,” said Adam Friedman, MD, interim chair of the Department of Dermatology at the GW School of Medicine and Health Sciences and senior author on the study.
This current survey from an interdisciplinary team of dermatology and emergency medicine researchers, led by Emily Murphy, a research fellow in the GW Department of Dermatology, examines whether the field of dermatology has advanced in its bioterrorism preparedness.
The survey, disseminated via the ODAC Dermatology, Aesthetic & Surgical conference listserv, found that only 28.9% of respondents received training in disaster preparedness and response. The respondents to the survey frequently commented that they felt dermatologists should be prepared for bioterrorism-related cutaneous diseases, such as anthrax or smallpox-related diseases, as well as infections resulting from natural disasters.
Similar to the 2003 survey, the authors found that few dermatologists received adequate bioterrorism preparedness training. Even among those who had reported training, many indicated they felt ill prepared to manage patients affected by disasters, especially biological attacks and nuclear or radiological events.
“While few respondents to the survey were trained in disaster preparedness, it is encouraging that 75% reported that it should be included in dermatology training,” Friedman said. “It is a necessary tool to advance the field.”
James Phillips, MD, section chief of disaster and operational medicine in the GW Department of Emergency Medicine, director of the GW Disaster Medicine Fellowship, and co-author on the study, agreed: “My fellows and I found great value in partnering with our dermatology colleagues for this project. It is my firm belief that, while disaster medicine and emergency management primarily fall within the scope of emergency medicine and trauma surgery, education, and training for other specialties is of great value and is virtually unexplored. In an increasingly complex disaster environment, we welcome such research collaborations with other GW specialists.”
###
The article, titled “A Survey of Dermatologists’ Preparedness for Natural and Man-made Disasters,” is published in the Journal of Drugs in Dermatology and can be found at jddonline.com/articles/dermatology/S1545961620P0016X/1.

Source: Next Steps in Dermatology
At the 17th Annual ODAC Dermatology, Aesthetic, and Surgical Conference (ODAC) held January 17-20 in Orlando, FL, Dr. Desiree Ratner led a discussion on new and emerging therapies for advanced non-melanoma skin cancer discussion.
Treatment Options
The session covered several treatments for patients including patidegib gel 2% and 4% applied once or twice daily in patients with basal cell carcinoma. Patidegib is a topical hedgehog inhibitor made by PellePharm and its mechanism of action is to block Smo signaling, thereby inhibiting the hedgehog pathway that contributes to the development of basal cell carcinomas. This treatment has several advantages in that it does not contribute to hair loss, taste loss, or muscle cramps. It has the potential to treat and mitigate facial basal cell carcinomas in basal cell nevus patients. It is being studied in randomized clinical trials enrolling patients with Gorlin’s syndrome (basal cell nevus syndrome) in the United States and in Europe.
Hedgehog pathway inhibitor resistance is unusual but may occur as “rebound” tumor growth after drug cessation or secondarily after long-term smoothened inhibitor therapy. Resistance to hedgehog pathway inhibitors is classified into primary and secondary resistance. Primary resistance has been postulated to bypass mechanisms of genes downstream of smoothened, such as the G497 W mutation. Secondary resistance in patients who showed an initial response has actually been thought to be due to de novo mutations located on regions in smoothened to which hedgehog pathway inhibitors bind or selective clonal expansion of minority clones in the pre-treated tumor. Further studies are definitely needed to elucidate what drives resistance to hedgehog pathway inhibitors and how basal cell carcinoma resistance may be overcome by other novel, emerging therapies.
Patient Cases
Dr. Ratner presented a number of interesting patient cases with advanced basal cell carcinomas sometimes so large that patients lose mobility and function of a body part or organ. In most cases, locally advanced BCCs respond well to oral hedgehog inhibitors, which can be used for long-term control or neoadjuvantly prior to surgery. In the case of one patient, an aggressive orbital BCC caused contraction of the tissues around his eye, such that he was not able to open it. Despite treatment with an oral hedgehog inhibitor, his tumor continued to grow, resulting in destruction of his orbit and locoregional metastasis.
Samples of his tumor and normal skin were sent to Stanford University, which performed whole exome sequencing. In the studies of these samples, it became evident that the tumor should have responded to vismodegib but had developed resistance due to another as yet unknown mechanism. Therapies designed to override resistance such as second-generation smoothened inhibitors are under development.

Source: The Dermatologist
The following is an excerpt from The Dermatologist as coverage from ODAC Dermatology, Aesthetic & Surgical 2020 where Sailesh Konda, MD, and Vishal Patel, MD, reviewed the guidelines and discussed considerations for when and when not to perform MMS.
Mohs micrographic surgery (MMS) is considered the gold standard of treatment for many skin cancers. However, this option is not always appropriate for every situation and every patient. Several factors should be considered when determining which option to use, including tumor size, patient age, and aesthetic outcomes, for treating skin cancer.
The Dermatologist: What are the guidelines for determining what tumors should and should not be treated with MMS?
Dr Konda: The appropriate use criteria (AUC) for MMS was developed in 2012 by an ad hoc task force.2 In general, MMS may be considered as a treatment option for tumors on the head, neck, hands, feet, pretibial surface, ankles, and genitalia; aggressive tumors of any location; tumors greater than 2 cm on trunk or extremities; recurrent tumors, and tumors arising in patients with a history of immunosuppression, radiation, or genetic syndromes.
An AUC score is assigned to tumors based on their characteristics. Tumors with scores of 7 to 9 are appropriate, 4 to 6 are uncertain (in extenuating circumstances, MMS may be considered), and 1 to 3 are inappropriate.
However, practitioners should remember that these are only guidelines! Even if a tumor meets criteria for MMS, the physician and patient should still discuss all available treatment options—both surgical and nonsurgical— and take into consideration associated cure rates; long-term clinical and aesthetic outcome; the patient’s age and comorbidities; and risks, benefits, and adverse effects before deciding on a treatment.
The Dermatologist: What tumors often deemed appropriate for MMS might not actually require MMS, and why?
Dr Konda: Superficial basal cell carcinoma and squamous cell carcinoma in situ are tumors that have been deemed appropriate for MMS. However, these tumors may also be treated with topical therapy (imiquimod and 5-fluorouracil), local destruction, fusiform or disc excision, photodynamic therapy, and lasers (CO2 +/- diode for follicular extension). These treatment modalities may provide cure rates lower than but approaching those of MMS, and may be preferred by physicians and patients in certain circumstances. When discussing treatment options, patients should be made aware of any therapies that may be used off-label or are not FDA-approved.
Additionally, lentigo maligna (melanoma in situ) and lentigo maligna melanoma may be treated with either MMS (frozen sections), staged excision with central debulk and complete margin assessment (permanent sections), or wide local excision (permanent sections).

Source: Dermatology News
The following is an excerpt from Dermatology News Expert Analysis, Conference Coverage from ODAC.
ORLANDO – Dermatologists should be well versed in addressing common concerns that patients, family members, and the media have about photoprotection, Adam Friedman, MD, advised at the ODAC Dermatology, Aesthetic, & Surgical Conference.
“Know the controversies. Be armed and ready when these patients come to your office with questions,” Dr. Friedman, professor and interim chair of dermatology at George Washington University, Washington, said in an interview at the meeting, where he presented on issues related to photoprotection.
Which SPF to choose and the impact of sunscreen on vitamin D are among the issues patients may be asking about. Sunscreen SPFs above 50 don’t technically provide a “meaningful” increase in ultraviolet protection, given that this value relates to filtering about 98% of UVB, but they still can provide some benefit, which has to do with real-world human error, Dr. Friedman said.

Source: Dermatology News
The following is an excerpt from Dermatology News Expert Analysis, Conference Coverage from ODAC.
ORLANDO – Because Food and Drug Administration–approved treatment options for children and adolescents with severe dermatologic diseases are limited, systemic therapies for these patients often require the use of off-label medications. However, this scenario is changing, A. Yasmine Kirkorian, MD, said at the ODAC Dermatology, Aesthetic & Surgical Conference.
“I really would like to emphasize that children with severe disease need to be treated,” added Dr. Kirkorian, a pediatric dermatologist at George Washington University, Washington, and Children’s National Health System, where she is interim chief of the division of dermatology.
Current on-label systemic therapies for pediatric skin disease include etanercept for psoriasis (4 years and older), ustekinumab for psoriasis (12 years and older), adalimumab for hidradenitis suppurativa (12 years and older), and omalizumab for chronic idiopathic urticaria (12 years and older). A new addition to the list is dupilumab, which was approved for children and adolescents with atopic dermatitis (AD) aged 12 years and older in 2019, she noted.

Source: The Dermatologist
The following is an excerpt from The Dermatologist article on Q&A with ODAC Dermatology, Aesthetic and Surgical conference faculty, Terrence Keaney, MD.
More and more men are seeking cosmetic procedures to improve their appearance and slow the aging process. In addition to anatomical differences, men have different concerns about how they look compared with women. Terrence Keaney, MD, discussed these concerns and trends among male aesthetic patients, and also shared pearls for treating this patient population at ODAC Dermatology, Aesthetic and Surgical conference in Orlando, FL.
Dr Keaney is founder and director of SkinDC and an assistant clinical professor of dermatology at George Washington University School of Medicine.
The Dermatologist: What are some common trends among male aesthetic patients?
Dr Keaney: Like broader trends in aesthetics, there is no cookie cutter technique for treating men. Gender is just one data point, albeit a fairly important one because it affects biology, anatomy, behavioral expectations, etc. When evaluating a new cosmetic patient, gender, age, ethnicity, and other patient factors play a role in creating a customized treatment plan.
Understanding aesthetic procedures among male patients has not been well-studied and has not been on the top of many aesthetic providers minds, most likely because men occupy a smaller percentage of cosmetic patients. However, the number of men seeking minimally invasive procedures is growing.
As more men seek cosmetic treatment, it is important that physicians and practitioners know how to approach these patients from a treatment perspective, as well as how to discuss complications from these procedures because these scenarios may be different compared with female patients.
The Dermatologist: What are some of the differences between male and female patients that dermatologists should keep in mind?
Dr Keaney: The number one difference between men and women is anatomy. Anatomy really dictates how a provider will perform a procedure, especially fillers.
The facial anatomy of men is very different than women. For example, the distribution of fat is different between the sexes. Men have less subcutaneous fat in the face, especially in the medial cheeks and middle of the cheek, and do not have high cheekbones, which dictates where a filler would be placed. The apex of the cheek tends to be lower and more towards the middle in men, whereas the apex tends to be high and lateral in women and is considered a very feminine feature.
Behaviors, such as goals and expectations of cosmetic procedures, differ between men and women as well. Men care about different factors than women. Specifically, men worry about 3 areas: the hairline, eyeline, and jawline. When discussing aesthetic procedures and performing a full-face analysis of male patients, I often refer back to these 3 areas because I know men tend to worry about them the most.
However, this does not mean I do not use fillers on the cheeks or the mid-face. When I use a filler, I explain to the patient so they understand how this procedure may influence how their jaw looks or their eyes look. Otherwise, they may not be interested in that treatment option.
Other major concerns among men include hair loss and body contouring.

Source: Next Steps in Derm
At the 17th ODAC -Aesthetic, Surgical and Clinical Dermatology Conference held January 17-20, 2020 in Orlando, FL, Dr. Angelo Landriscina led a session on developing new approaches to caring for LGBTQ+ patients.
Next Steps correspondent Dr. Anna Chacon reports back on highlights and pearls from the session which covered the following:
Why this topic?
Updating Our Understanding of SGM Patients
Caring for Transgender Patients
Aesthetic Treatments for Transgender Patients
Creating A Competent Clinical Environment
Why this topic?
It is difficult to determine how many people identify as LGTBQ+ in the United States. Right now, our best estimate is about 4% based on survey data. These patients tend to cluster into different areas, but it’s likely that you will see 2-3 patients per day who are a part of these communities.
Using the appropriate terminology is also key. There is a difference between sexual orientation and gender identity. Sexual orientation describes an individual’s emotional, romantic or sexual attraction to others while gender identity can be male, female or neither, and it can change over time.
What does LGTBQ+ stand for?
The acronym stands for lesbian, gay, bisexual, transgender, queer and questioning but can even be longer (LGBTQQ2SIAA)! There are other terminologies that can also be included such as intersex, gender fluid, and gender queer. Intersex describes: a variation in sex characteristics including chromosomes, gonads, or genitals that do not allow an individual to be distinctly identified as male or female. Gender fluid describes a person who doesn’t identify with a fixed gender at all times. And genderqueer is an umbrella term for gender identities that are not exclusively masculine or feminine identities which are thus outside of the gender binary and cisnormativity.
Queer is a blanket term that can describe all of these but has a loaded history since it used to be use as a slur. SGM stands for sexual and gender minority, which is an easy clinical and scientific term to use when talking about this population. While it is helpful to become familiar with the appropriate terminology, it is also important to be mindful of which particular terms to avoid when talking to patients such as: homosexual, sexual preference, “lifestyle,” and “sex change.”.
When it comes to pronouns, it is best to ask patients which they prefer. In situations where this may be unclear, the singular pronoun “they” may be your best friend – it was Merriam-Webster’s 2019 word of the year!
Additional tips for the dermatologist include being comfortable with not knowing everything, allowing your patients to define themselves, and recognizing that sexual orientation and gender identity are independent of each other.
Source: Next Steps in Derm
Dermoscopy, also known as epiluminescence microscopy, epiluminoscopy or skin surface microscopy, is an important way to visualize subsurface structures in the epidermis and dermis. In a 2-part series, Dr. Sima Jain reviews the evaluation of pigmented lesions, and the different vessel morphologies and patterns along with a discussion of specific findings in select cutaneous infections.
Read part 1 here
Read part 2 here
If you want to learn more about dermoscopy, make sure to register for the upcoming ODAC Dermatology, Aesthetic & Surgical Conference where Dr. Sima Jain will lead the following dermoscopy sessions:
During this session, Dr. Jain will present challenging clinical cases and explore how dermoscopic evaluation can significantly increase clinical acumen.
Attendees will:
Perifollicular scaling and fibrotic white dots are seen in lichen planopilaris. Orthogonal white streaks can be seen in melanoma. Glomerular vessels are often seen in Bowen’s disease.
During this session, Dr. Jain will review the basics of dermoscopy and how it can be used to help diagnose both pigmented and non-pigmented skin lesions.
Attendees will:
White streaks can be seen in melanoma and basal cell carcinoma. Telangiectasias, leaf-like areas and spoke wheel pigmentation are seen in basal cell carcinomas. The delta wing jet with contrail is specific for scabies.

Source: Practical Dermatology
Susan Weinkle, MD, has been awarded the Outstanding Educator and Mentor in Dermatology Award by the ODAC Dermatology, Aesthetics & Surgical Conference, in partnership with the Journal of Drugs in Dermatology (JDD).
The award recognizes Dr. Weinkle for her long-standing commitment to educating and mentoring the next generation of dermatologists and for devoting a major portion of her professional life to enhancing the practice and profession of dermatology through education.
“Susan has given all of us in aesthetics so much of her time and energy, and I am honored to present this award to her.”“It is a pleasure and an honor to recognize the tireless work of exceptional leaders in dermatology,” said Shelley Tanner, CEO and president of SanovaWorks, which produces the JDD, ODAC, Derm In-Review, and Next Steps in Dermatology. “Not only do these dermatology leaders dedicate their entire lives to benefiting patients every day, but after the ‘work day’ ends, they spend countless hours involved in activities to improve the specialty’s future. We congratulate Dr. Weinkle for being chosen for this award.”

Source: DermatologyTimes
A south Florida practitioner’s contribution to dermatology is not going unnoticed at the 2020 Orlando Dermatology, Aesthetic & Surgical Conference (ODAC) with the recent presentation of the Journal of Drugs in Dermatology (JDD) Outstanding Educator & Mentor in Dermatology Award to Susan Weinkle, M.D, Tampa, Fla.
Dr. Weinkle, an assistant clinical professor of dermatology at the University of South Florida, was recognized for her dedication to mentoring and educating future dermatologists, and commitment to advancing the dermatology industry through education.
Aside from being an educator, Dr. Weinkle specializes in cosmetic surgery and Mohs Micrographic Surgery at her private practice in Bradenton, Fla.
She was also the president of the American Society for Dermatological Surgery and the Women’s Dermatological Society. Additionally, she was previously a committee chair and board of directors member at numerous dermatology organizations including the Florida Society of Dermatology and Dermatologic Surgery, American Academy of Dermatology and Dermatology Foundation.

Source: SanovaWorks
NEW YORK – Erik J. Stratman, MD, 2019 President of the American Board of Dermatology (ABD), to present on Maintenance of Certification (MOC) CertLink in January at ODAC Dermatology, Aesthetic and Surgical conference.
Changes to MOC
A major shift in continuing certification is coming for board-certified dermatologists in January. Erik J. Stratman, MD will present, “Changes to Your MOC Requirements: What Every Dermatologist Should Know about CertLink,” on January 17th, 2020 at the J.W. Marriot in Orlando, Florida.
Workshop Description
Dr. Stratman will walk-through the CertLink® MOC program and demonstrate its design, rationale and navigation. According to the ABD, CertLink provides the utmost flexibility in MOC and provides an alternative to the one-time, sit-down, high stakes in-person MOC examination. Dermatologists will be able to go online and take test questions in the convenience of their own home or office at various times throughout the year.
ABD MOC CertLink®
CertLink® is a longitudinal testing platform. The platform is designed to test and build medical knowledge in a “test to competence” type model. In addition, CertLink® will keep dermatologists up to date by providing the latest articles from dermatology subspecialties. CertLink™ assessment platform is powered by American Board of Medical Specialties (ABMS).
Registration and Fees
The pre-conference workshop is provided complimentary for dermatologists registered for ODAC 2020.
About ODAC
Attend ODAC to stay connected, informed, and up-to-date in dermatology. ODAC (previously Orlando Derm) is one of the largest and most prestigious conferences of the year. ODAC attracts a national audience of over 650 US Dermatology Physicians, Dermatology Residents, Nurse Practitioners and Physician Assistants.
Visit orlandoderm.org to register for ODAC and attend this workshop. ODAC is a product of SanovaWorks.

Source: Next Steps in Dermatology
ODAC speaker, Sima Jain, MD provides a two-part series on Hormonal Acne for Next Steps in Derm.
Dermatologists should be able to distinguish which patients presenting with acne may need further evaluation for a possible underlying endocrinopathy. In this two-part series, Dr. Jain will be focuses on hormonal acne specifically related to PCOS, including the exam, work up, diagnosis, treatment and long-term implications of this syndrome.
PCOS is a complex disorder affecting 5-10% of reproductive-age women and is characterized by a state of hyperandrogenism and often hyperinsulinemia. It is the most common endocrine disorder in women and is a major cause of infertility due to lack of ovulation. Patients can present with a wide range of symptoms, which may make the precise diagnosis difficult.
Acne is a common skin manifestation but other potential findings may include hirsutism (increased terminal hairs in a male-pattern distribution, scalp alopecia, acanthosis nigricans and less frequently seborrheic dermatitis. Non-dermatologic symptoms and signs may include irregular menses (oligomenorrhea), insulin resistance, polycystic ovaries and infertility.
Since a dermatologist may be the first or only physician a young female patient with hormonal acne sees, it is imperative for us to be aware of the clinical clues that suggest hyperandrogenism. First, it is important to inquire if the patient’s menstrual cycles are regular to screen for oligomenorrhea and potential anovulation. Be mindful if the patient is on an oral contraceptive pill, as this can mask underlying oligomenorrhea since the external hormones are essentially regulating the menstrual cycle. In addition to discussing the menstrual history, it is important to inquire about potential hirsutism by asking if the patient has noticed increased hair growth to the face (sideburn area, chin, upper cutaneous lip), chest, abdomen and/or inner thighs. Many patients do not realize that increased hair growth may be related to acne and often feel embarrassed to bring it up on their own. A third important feature to be aware of is hair loss to the scalp. It is not uncommon for patients to say they have noticed thinning of their hair or increased shedding, especially to the front of their scalp.
Visit Next Steps in Derm to read the series or attend ODAC to learn more.
Source: Next Steps in Dermatology
ODAC speaker, Sima Jain, MD provides a two-part series on Hormonal Acne for Next Steps in Derm.
Dermatologists should be able to distinguish which patients presenting with acne may need further evaluation for a possible underlying endocrinopathy. In this two-part series, Dr. Jain will be focuses on hormonal acne specifically related to PCOS, including the exam, work up, diagnosis, treatment and long-term implications of this syndrome.
PCOS is a complex disorder affecting 5-10% of reproductive-age women and is characterized by a state of hyperandrogenism and often hyperinsulinemia. It is the most common endocrine disorder in women and is a major cause of infertility due to lack of ovulation. Patients can present with a wide range of symptoms, which may make the precise diagnosis difficult.
Acne is a common skin manifestation but other potential findings may include hirsutism (increased terminal hairs in a male-pattern distribution, scalp alopecia, acanthosis nigricans and less frequently seborrheic dermatitis. Non-dermatologic symptoms and signs may include irregular menses (oligomenorrhea), insulin resistance, polycystic ovaries and infertility.
Since a dermatologist may be the first or only physician a young female patient with hormonal acne sees, it is imperative for us to be aware of the clinical clues that suggest hyperandrogenism. First, it is important to inquire if the patient’s menstrual cycles are regular to screen for oligomenorrhea and potential anovulation. Be mindful if the patient is on an oral contraceptive pill, as this can mask underlying oligomenorrhea since the external hormones are essentially regulating the menstrual cycle. In addition to discussing the menstrual history, it is important to inquire about potential hirsutism by asking if the patient has noticed increased hair growth to the face (sideburn area, chin, upper cutaneous lip), chest, abdomen and/or inner thighs. Many patients do not realize that increased hair growth may be related to acne and often feel embarrassed to bring it up on their own. A third important feature to be aware of is hair loss to the scalp. It is not uncommon for patients to say they have noticed thinning of their hair or increased shedding, especially to the front of their scalp.
Visit Next Steps in Derm to read the full series or attend ODAC to learn more.

Source: Next Steps in Dermatology
Health recently wrote an article asking if CBD oil can relieve psoriasis symptoms.
In recognition of Psoriasis Awareness Month, I consulted Adam Friedman, MD, FAAD, professor and interim chair of dermatology at the George Washington School of Medicine and Health Sciences. Dr. Friedman is also the residency program director, director of translational research and director of the Supportive Oncodermatology Clinic. In addition, Dr. Friedman serves as Medical Director for ODAC -Dermatology, Aesthetic & Surgical Conference.
We have only begun to scratch the surface of the unbridled potential of cannabinoids as therapeutic agents. Interestingly enough, psoriasis is one of the listed indications for medical cannabis in the great state of Connecticut, though little is really known on this and many other spaces in dermatology.
Let’s take a step back and first talk about CBD. CBD stands for cannabidiol, one of about 120 different molecules that come from the cannabis plant. It’s the second most prevalent active ingredient in cannabis – tetrahydrocannabinol (THC) is the first. But unlike other cannabinoids – such as THC — CBD does not produce a euphoric “high” or psychoactive effect. That said, it has tremendous biological reactivity through binding to a multitude of receptors, including the cannabinoid specific receptor, CB2r, which is expressed by practically every immune cell (as opposed to CB1r, which is most heavily expressed in the peripheral and central nervous system), regulating skin physiology by being anti-inflammatory, lipostatic and antiproliferative.
Now back to the original question. Inflammatory skin conditions such as psoriasis result from a number of aberrant responses of the immune cells and immune signaling in the skin. Looking at psoriasis specifically, dysregulation of the skin immune system results in marked proliferation and keratinization of epidermal cells. Overactivation of Th1 and Th17 inflammatory responses in psoriasis produces cytokines like IL-17 and IL-22 that set off cascades of events resulting in increased keratinocyte proliferation, expression of keratins 6 and 16, and inflammatory cell infiltration. Because of its role in regulating the inflammatory response of keratinocytes and dermal immune cells, the endocannabinoid system offers potential targets for the management of many inflammatoryskin conditions, but the data to date is rather limited, mostly to cell bases, ex vivo and animal models.
This is what we know:Activation of the endocannabinoid system in the skin reduces inflammation through a number of mechanisms, such as shifting the pro-inflammatory Th1 response to an anti-inflammatory Th2 response via CB2r activation (thank you, CBD). The endocannabinoid system also plays a role in regulating keratinocyte proliferation and differentiation, which are pathologically increased in psoriasis. For example, CB1r activation by cannabinoids such as anandamide (AEA) inhibits keratinocyte differentiation and decreases production of keratin K6, a marker of keratinocyte hyperproliferation. The potential therapeutic effects of CBD in psoriasis also include activation of non-cannabinoid receptors such as GPR55, which reduces inflammation caused by nerve growth factor, and PPARα and PPARγ which reduces epidermal hyperplasia via suppressed proliferation of keratinocytes.

Dermatologists are well aware of the difficulty in managing itchy patients. Itch can be caused by a number of cutaneous and extracutaneous diseases. Regardless of the etiology, itch is one of the most frustrating symptoms of patients and management dilemmas for dermatologists. At the 16th Annual ODAC conference, Dr. Brian Berman reviewed some of the emerging therapies for the treatment of itch and the etiologies for which they are currently under investigation.
Nemolizumab is a monoclonal antibody directed at the IL-31 receptor A. It is currently being studied for use in atopic dermatitis. Recent phase II data have shown improvement for itch in atopic dermatitis over 64 weeks1. A few of the less common side effects that were seen in this study included peripheral edema and elevations in blood CPK levels.
Tapinarof cream is a first-in-class, naturally derived, non-steroidal topical agent. It is currently being investigated for use in psoriasis and atopic dermatitis. Tapinarof is a therapeutic aryl hydrocarbon modulating agent (or TAMA) and inhibits specific proinflammatory mediators, including IL-6 and IL-17A2. One of the more interesting targets of tapinarof is nuclear factor-erythroid 2-related factor-2 (Nrf2), which happens to be one of the mechanisms through which coal tar produces its beneficial effects.
Hypochlorous acid gel is being used for its anti-inflammatory properties. This topical has potential utility for atopic and seborrheic dermatitis-related itch.
Serlopitant is an oral NK1 receptor antagonist. It is currently being investigated for use in chronic pruritus, pruritus in psoriasis, and prurigo nodularis. Substance P binds to the NK1 receptor peripherally, in the ganglion and brain to cause/increase the perception of itch, and as such, NK1 receptor antagonists are an up and coming mechanistic target for itch. Phase II data appear to be promising3.
Remetinostat (previously referred to as SHAPE), a topical histone deacetylase inhibitor, is currently under investigation for treating pruritus in patients with stage IA-IIA mycosis fungoides4. Preliminary data are promising as the topical route of the medication appears to decrease itch while limiting side effects compared to systemic histone deacetylase inhibitors.
Omalizumab, an anti-IgE monoclonal antibody, is approved for use for chronic idiopathic or chronic spontaneous urticaria5. It is notable that in the pivotal, phase 3 study published in the New England Journal of Medicine, the primary endpoint was itch-severity score rather than urticarial lesion counts. The use of this endpoint highlights the magnitude of itch in urticaria.

Dermatology thought leader Hilary Baldwin, MD helps us make sense of cosmeceuticals by sharing her approach to them, including how to define them and evaluate their utility.
On a funny note, Dr. Baldwin confesses being a skeptic and a hypocrite when it comes to cosmeceuticals. She remains skeptical about some of the science but at the same time uses 5 cosmeceutical products herself. We love her honesty!
The term was accredited to Albert Kilgman in 1984 as the ill-defined realm between cosmetics and prescription skincare products. Like a cosmetic, it is topically applied; like a drug, it contains ingredients that influence biologic functioning of the skin.
Fortunately for the FDA, they have no comment (and we would prefer to keep it that way!). Cosmetic companies consider them to be well-studied actives with proven efficacy. For most dermatologists, they are not well studied, they have some data behind them and are products that may or may not live up to claims (some of which are quite grandiose!). Cosmeticdermatologists on the other hand, feel a little bit different and think these are products that may alter wound healing and may prolong the effects of cosmetic procedures. Patients, however, consider cosmeceuticals to be miracle cures, which Dr. Baldwin believes is the problem and where a disconnect exists. In the quest for medical cures, we don’t want patients to be dissatisfied and frustrated…and poor. It is unlikely that topicals, or at least a single topical, can fully address the complex process and major issues that causes the aging appearance, such as:
Dr. Baldwin notes that when patients come into the office, they have a couple of specific requests: “Do I need a face lift yet?”, “What can you do to fix my face?”. Sometimes they even ask if there is some magic cream they can put on their face to make them look less tired. Dr. Baldwin suggests to her patients to think of their face as an old couch in their living room that they no longer care for. Do they no longer care for it because it is sagging and actually has structural abnormalities, or do they not like it because the slipcovers are torn and stained? When we talk about cosmeceuticals, what we are talking about is slipcover repair, we are not talking about sagging skin because cosmeceuticals may be able to handle the drying on the sofa but they are not going to help with the sagging of the sofa.
The average U.S. woman uses 15 different cosmetic products each day. If you figure that each of them contains 10-50 ingredients, the average woman is putting an awful lot of chemicals on her face every day, and it should be something that actually works, is safe, and non-irritating.
The truth is that patients dolike to use cosmeceuticals as feel they are doing something for themselves. Cosmeceuticals can make retinoids more tolerable and effective and can prolong or improve the results of cosmetic procedures.
Dr. Baldwin believes it is the job of dermatologists to help patients make reasonable choices and manage their expectations. How often does a patient come to you with a bunch of pieces of papers from magazines and newspapers and ask you about all these miracle cures? Or bring you a before and after picture saying, “Look at how much better she looks in the after picture” which is clearly a photographic cure, or perhapsthere is actually a cure there, but we can make no judgements based on these photographs which are just rampantin the magazines patients are looking at.
The fear of wrinkles, coupled with the fear of procedures, make some of Dr. Baldwin’s patients say that “they are looking for something better than Botox”. But is there a topical that is superior to fillers and neuromodulating agents? The magazines say there is…so it must be true, and then we have “friends” in the media who tell us every day there are products out there, one on Monday, a completely different one on Tuesday, yet a different one on Wednesday that will be life changing.

Source: Next Steps in Dermatology
Dermatologists are well aware of the difficulty in managing itchy patients. Itch can be caused by a number of cutaneous and extracutaneous diseases. Regardless of the etiology, itch is one of the most frustrating symptoms of patients and management dilemmas for dermatologists. At the 16th Annual ODAC conference, Dr. Brian Berman reviewed some of the emerging therapies for the treatment of itch and the etiologies for which they are currently under investigation.
Nemolizumab is a monoclonal antibody directed at the IL-31 receptor A. It is currently being studied for use in atopic dermatitis. Recent phase II data have shown improvement for itch in atopic dermatitis over 64 weeks1. A few of the less common side effects that were seen in this study included peripheral edema and elevations in blood CPK levels.
Tapinarof cream is a first-in-class, naturally derived, non-steroidal topical agent. It is currently being investigated for use in psoriasis and atopic dermatitis. Tapinarof is a therapeutic aryl hydrocarbon modulating agent (or TAMA) and inhibits specific proinflammatory mediators, including IL-6 and IL-17A2. One of the more interesting targets of tapinarof is nuclear factor-erythroid 2-related factor-2 (Nrf2), which happens to be one of the mechanisms through which coal tar produces its beneficial effects.
Hypochlorous acid gel is being used for its anti-inflammatory properties. This topical has potential utility for atopic and seborrheic dermatitis-related itch.
Serlopitant is an oral NK1 receptor antagonist. It is currently being investigated for use in chronic pruritus, pruritus in psoriasis, and prurigo nodularis. Substance P binds to the NK1 receptor peripherally, in the ganglion and brain to cause/increase the perception of itch, and as such, NK1 receptor antagonists are an up and coming mechanistic target for itch. Phase II data appear to be promising3.
Remetinostat (previously referred to as SHAPE), a topical histone deacetylase inhibitor, is currently under investigation for treating pruritus in patients with stage IA-IIA mycosis fungoides4. Preliminary data are promising as the topical route of the medication appears to decrease itch while limiting side effects compared to systemic histone deacetylase inhibitors.
Omalizumab, an anti-IgE monoclonal antibody, is approved for use for chronic idiopathic or chronic spontaneous urticaria5. It is notable that in the pivotal, phase 3 study published in the New England Journal of Medicine, the primary endpoint was itch-severity score rather than urticarial lesion counts. The use of this endpoint highlights the magnitude of itch in urticaria.
Physician assurance reduces itch. In a recent study6, a physician administered a histamine skin prick to 76 participants. After 3 minutes, half of the randomly selected participants were assured by the physician in the following way. “From this point forward your allergic reaction will start to diminish, and your rash and irritation will go away.” In the assured group, it was found that over the next 15 minutes, itchiness of the area declined significantly faster than the group not assured by the physician.
Source: Next Steps in Derm
Backed by a mountain of evidence, Dr. Zitelli walked us through the new and changing role of sentinel lymph node biopsy for melanoma in a riveting 20-minute talk presented at the 16th annual ODAC conference. Here are the highlights.
Before delving in, Dr. Zitelli skillfully laid the framework for his lecture. The crux of sentinel lymph node biopsy is based on the theory of orderly progression, in which malignant melanoma cells leave the tumor and preferentially enter the lymphatics and the first lymph node. This theory is rivaled by the anatomic pathway, in which malignant melanoma cells may enter the lymphatics or the blood stream, resulting in simultaneous dissemination.
The overwhelming preponderance of evidence supports the latter anatomic theory – melanoma cells may enter the blood stream directly or the lymphatics, potentially bypassing the sentinel node. This anatomic theory is evidence based. It refutes the theory of orderly progression that the concept of sentinel lymph node biopsy is based on. Another common misconception is that lymph nodes are filters – they are not. Lymph nodes are sampling organs, sampling antigens in order to initiate an immune response.
With the groundwork laid, Dr. Zitelli went on to summarize the emerging evidence for sentinel lymph node biopsy. “This is what you need to know when you counsel a patient in order to obtain true informed consent.”
What you’ve been told: Sentinel lymph node biopsy improves survival
What the evidence shows: There is not a single solid tumor for which sentinel lymph node biopsy has been shown to provide a survival benefit.
We’ve been told that sentinel lymph node biopsy improves survival in intermediate thickness melanoma, because subclinical deposits are removed from the lymph nodes before they can grow. In fact, 33% of patients who underwent sentinel lymph node biopsy, did so because they thought it would improve their survival. Yet, there is not a single solid tumor – melanoma, gastric, renal, thyroid or otherwise – where electively removing normal lymph nodes, even in the case of microscopic involvement, has shown a survival benefit.
A cornerstone trial, the Multicenter Selective Lymphadenectomy Trial (MSLT-1), set out to prove the survival benefit of sentinel lymph node biopsy in melanoma. However, sentinel lymph node biopsy failed to improve melanoma specific survival. Subsequently, MSLT-2 looked at whether removing positive lymph nodes further down the line would improve survival in patients who had positive sentinel lymph nodes – this was also a negative study.

Source: Next Steps in Derm
At the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL, longtime meeting Vice Chair Dr. Joel L. Cohen from Denver Colorado, spoke on perioral combination therapy. His presentation outlined his approach to perioral rejuvenation with one main theme – combination treatment, combination treatment, combination treatment. Simply put, combination treatment for perioral rejuvenation yields the most optimal results.
Dr. Cohen’s approach to perioral rejuvenation begins by dividing his work into its requisite parts. If the patient has excessive animation, toxins are recommended. If the patient has only a few superficial etched lines, fillers are recommended. If the patient has more significant or many perioral rhytides, laser resurfacing is the tool of choice – but he emphasizes full-field erbium over fractional options for significant etched-lines (see figure 1). Overall, all three should be considered individually or in combination to yield the best results. A major take home point regarding perioral rhytides is that fillers and toxins are not the primary treatment for this condition — and patients with etched-lines on the upper lip really need laser resurfacing.
His presentation also highlighted the need to address the entire perioral area when treating cutaneous lip etching – such as fillers in the nasolabial folds, antero-medial cheek, secondary smile lines, marionette area, and pre-jowl sulcus.
When addressing the mucosal lips as far as lip volume, it is of the utmost importance to make sure patients have a realistic expectation of results. Dr. Cohen prefers to use the Merz lip fullness scale, one of the scales that he co-authored. With this scale, no patient should jump from a zero to a four. Patients should move one or two grades on the scale in order to keep the result looking natural – and to be honest, it often isn’t even realistic for someone with really skinny lips to augment to full grade 4 lips, the anatomy just doesn’t accommodate that type of change.
It’s also important to note that mucosal lip-augmentation often results in neo-collagenesis over time. Therefore, it is important to get volume and proportions right in the first place, and not just simply squirt a lot of volume all over the lip or even uniformly throughout the lip. The medial lip should be fuller than the lateral lip. And the lip should have tubercles of projection points.

Source: Dermatology Times
Sentinel lymph node biopsy (SLNB) has classically been performed for regional disease control and to hopefully prevent disease metastasis; however, according to one expert, there has not been any good evidence to support this practice. As such, it is important for clinicians to focus on the evidence when planning the treatment and management of their advanced melanoma patients.
“Over the last decade or so, the role of SLNB has been changing, and there is no real consensus as to when to perform the procedure because it is a very rapidly changing field. The touted usefulness in survival benefit or prognosis of SLNB simply cannot be backed up by the available data, essentially rendering the appropriate use of SLNB in therapeutic limbo,” said John Zitelli, M.D., clinical associate professor, departments of dermatology & otolaryngology, University of Pittsburgh Medical Center, Pittsburgh, Penn., who spoke at the Orlando Dermatology and Aesthetic Conference.
According to Dr. Zitelli, the theory that SLNB would provide a survival benefit was debunked with the MSLT-1 research study1 recently published in the New England Journal of Medicine, and the idea that the procedure was to be considered as the most accurate prognostic test was also shown to be untrue. There usually is no need to do a SLNB, Dr. Zitelli said. The Breslow thickness, as well as all of the presenting clinical pathological morphologic features, such as ulceration of the tumor, is a wealth of information that the clinician can use to contemplate appropriate further treatment and management of the patient. Many clinicians still prefer to perform SLNB, Dr. Zitelli said, reasoning that waiting until the tumor is palpable would likely be synonymous with greater complications.
“The premise is off, because if you’re performing SLNB on a lot of people and the complication rate is low but the number of patients who are getting the procedure is high, the long-term complication rate in a group of people who you manage with SLNB actually have more complications than the smaller group of patients who have a complete node dissection from palpable disease,” Dr. Zitelli said.
Controversy revolving around the role of SLNB and its true usefulness in melanoma therapy and management continues today. The current contemporary wisdom is that SLNB should be performed because the results could help determine which patients would be more amenable to adjuvant therapy.
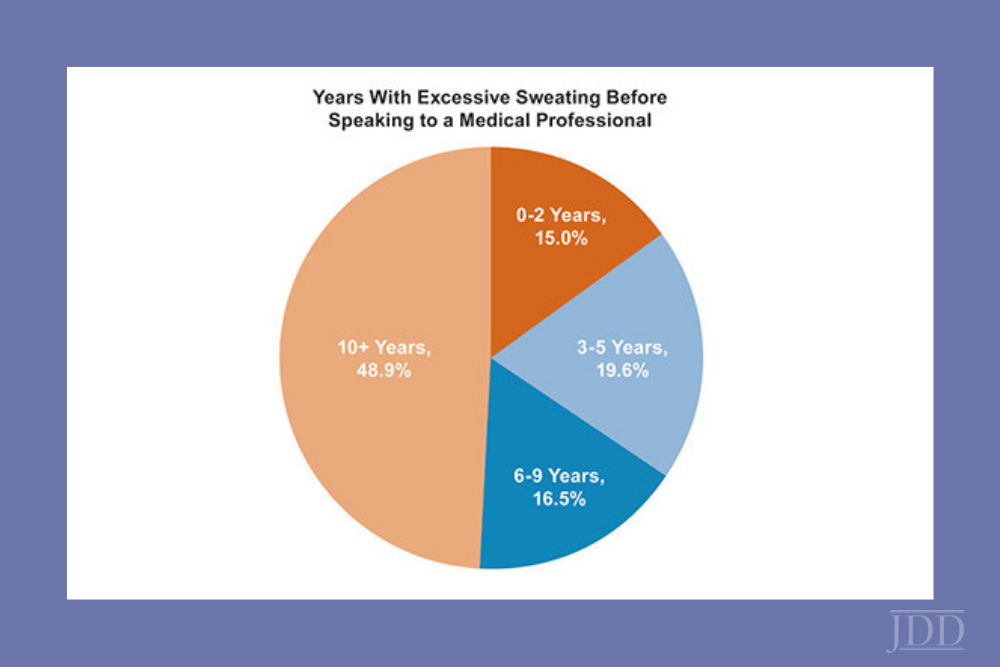
Source: Next Steps in Derm
Can you think of a skin condition that has a greater negative impact on quality of life than eczema or psoriasis? That’s right, you guess it—hyperhidrosis! I still remember my first hyperhidrosis patient who refused to shake people’s hands, go on dates, or attend social events due to his condition. After his treatment, he was like a new man. I can’t tell you how satisfying it was to see his life changed after treatment. That’s why I’m so excited to share what I learned from Dr. Adam Friedman at ODAC 2019 regarding hyperhidrosis. Dr. Adam Friedman is Professor and Interim Chair of Dermatology, Residency Program Director, Director of Translational Research, and Director of the Supportive Oncodermatology Clinic in the Department of Dermatology at The George Washington University School of Medicine & Health Sciences.
Nearly 5% of the world’s population suffers from hyperhidrosis—that’s 365 million people worldwide! In the U.S., 7.8 to 13.4 million people (2.8-4.8%) are estimated to be affected by hyperhidrosis—that’s comparable to the prevalence of psoriasis. Spalding et al. showed that patients with hyperhidrosis reported a worse quality of life compared to those with atopic dermatitis or psoriasis (Value in Health 2003). That made me raise my eyebrows for sure!
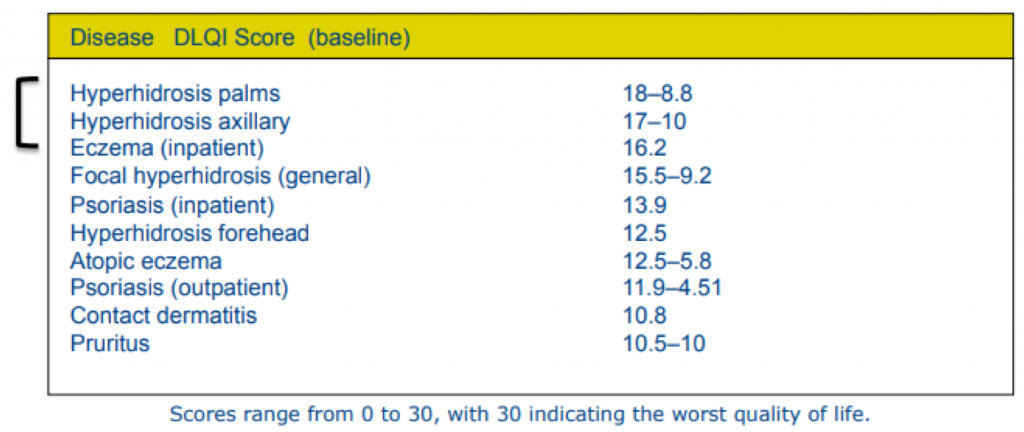
Hyperhidrosis can be divided into primary (usually focal) and secondary (generalized). For secondary hyperhidrosis, the underlying cause needs to be addressed, which may include drugs, cardiovascular disorders, respiratory failure, infections, malignancies, and metabolic disorders. For primary hyperhidrosis, now, that’s where we dermatologists step in and save the day. So, what are our options?
There are non-invasive, minimally invasive, and surgical options for the treatment of hyperhidrosis. Here, we will discuss everything but surgical options and energy-based treatment.

Source: Next Steps in Derm
This information was presented by Dr. Adam Friedman at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL. The highlights from his lecture were written and compiled by Dr. InYoung Kim.
If you’re a coffee drinker, you may be relieved to know that there was an inverse association between caffeine intake and risk of rosacea in a recent study. That was a huge relief for me for sure! Unfortunately, we can’t prescribe caffeine for rosacea and call it a day. So, what works?
High-yield pearls on the pathophysiology and management of rosacea are shared by Dr. Adam Friedman – Professor and Interim Chair of Dermatology, Residency Program Director, Director of Translational Research, and Director of the Supportive Oncodermatology Clinic in the Department of Dermatology at The George Washington University School of Medicine & Health Sciences. Here are the highlights.
First, let’s talk about diagnosis. Rather than categorizing into 4 classic subtypes that we learned in the textbook, rosacea may be better defined by “phenotypes”. Diagnostic phenotypes include 1) having fixed centrofacial erythema in a characteristic pattern that may periodically intensify or 2) phymatous changes. In the absence of these, the presence of 2 or more major features may be diagnostic, including papules/pustules, flushing, telangiectasia, ocular symptoms. Some secondary phenotypes that may help with diagnosis are burning/stinging, edema, dry appearance, and ocular rosacea.
While rosacea has widely been considered a disorder selectively affecting the Caucasian population, this is not true! Perhaps due to this bias, delayed diagnosis has been reported in substantial numbers. In fact, the prevalence of rosacea in skin of color is as high as 10%! That is significant. Please spread the word! So how do they present differently than Caucasian patients? While you may not see the persistent facial erythema (which is common in whites), the granulomatous subtype and papules/pustules are more common in skin of color. Asking about the secondary phenotypes noted above (burning/stinging, edema, dry appearance, and ocular rosacea) may also be helpful in diagnosis.
While many prescription treatment options exist (outlined below), patient education concerning proper general skin care is of utmost importance. Make sure to include these in your counseling: daily sunscreen, gentle moisturizers, gentle cleansers, avoid triggers.
A list of FDA-approved topical therapies that you may choose from:
What would a typical daily plan look like for a moderate-to-severe rosacea patient? Here are Dr. Friedman’s tips:
Source: Next Steps in Derm
Dr. Deirdre Hooper, an expert aesthetic and medical dermatologist, discussed the emerging use of Platelet-rich Plasma in the treatment of alopecia and skin rejuvenation at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference. Dr. Nikhil Shyam shares his takeaways and pearls from this lecture.
Platelet-rich plasma (PRP) is rapidly gaining popularity amongst dermatologists for its potential use in treating hair loss, acne scarring and facial rejuvenation. However, there is significant variability in the processing of PRP and there are currently no established treatment protocols.
Overall, PRP is increasingly being utilized for hair loss, scarring and facial rejuvenation. Currently, PRP appears to be safe with no long-term side effects noted. It may be used synergistically with existing treatment options with added benefit. Further research is required to establish the optimal PRP processing technique and to establish standardized treatment protocols.
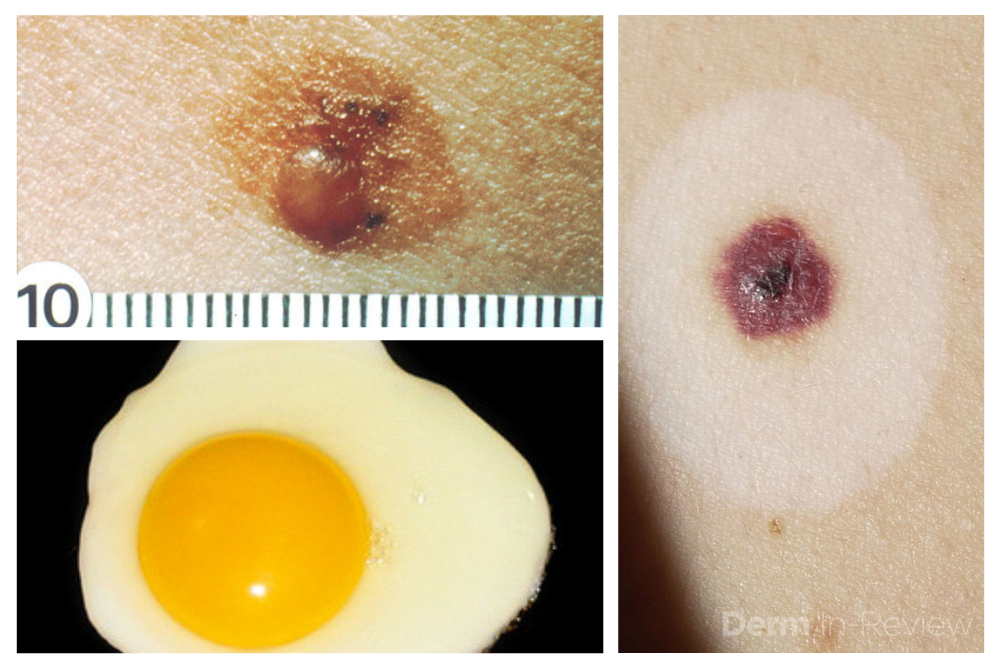
Source: Next Steps in Derm
This information was presented by Dr. Jean Bolognia at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL. The highlights from her lecture were written and compiled by Dr. Daniel Yanes.
Despite being one of the more common reasons for consulting a dermatologist, the diagnosis and management of atypical nevi remain nuanced and can often be challenging. I had the opportunity to learn from Dr. Jean Bolognia on her approach to atypical nevi, and walked away with many pearls to share.
Sometimes it can be overwhelming to know where to begin when tasked with the patient who has numerous and atypical nevi. The first step is to identify the patient’s signature nevus. Do they tend to grow fried egg nevi, eclipse nevi, or cockade nevi? Are their signature moles all pink with little brown pigment, or are they pitch black with a wafer of scale? Identifying the signature nevus assists in determining the ugly duckling, and it will also help you develop a practical approach. In addition, if the patient has primarily pink nevi, palpation for induration versus soft flabbiness is helpful as banal intradermal melanocytic nevi can be pink in color. If the patient has primarily small flat black nevi, you should hone in on the presence of inflammation that is not simply due to acne or folliculitis. Creating an individualized plan is the key to a successful examination.
In addition to identifying the signature nevus, it is also essential to understand how melanocytic nevi evolve over time. While nevi classically progress from junctional to compound and then to dermal, sometimes they simply fade away. In the case of fried egg nevi, the “yolk” becomes more raised and softer over time while the “white” of the egg gradually fades (figure 1). This results in multiple large dermal nevi on the trunk in an older patient. Patients can be taught that when a nevus elevates, determining if the lesion is firm versus soft can assist in distinguishing between the need for evaluation versus an aging phenomenon. Although not all changing nevi are concerning nevi, it is still essential to give the patient’s nevus of concern special attention, even if it doesn’t catch your eye at first.
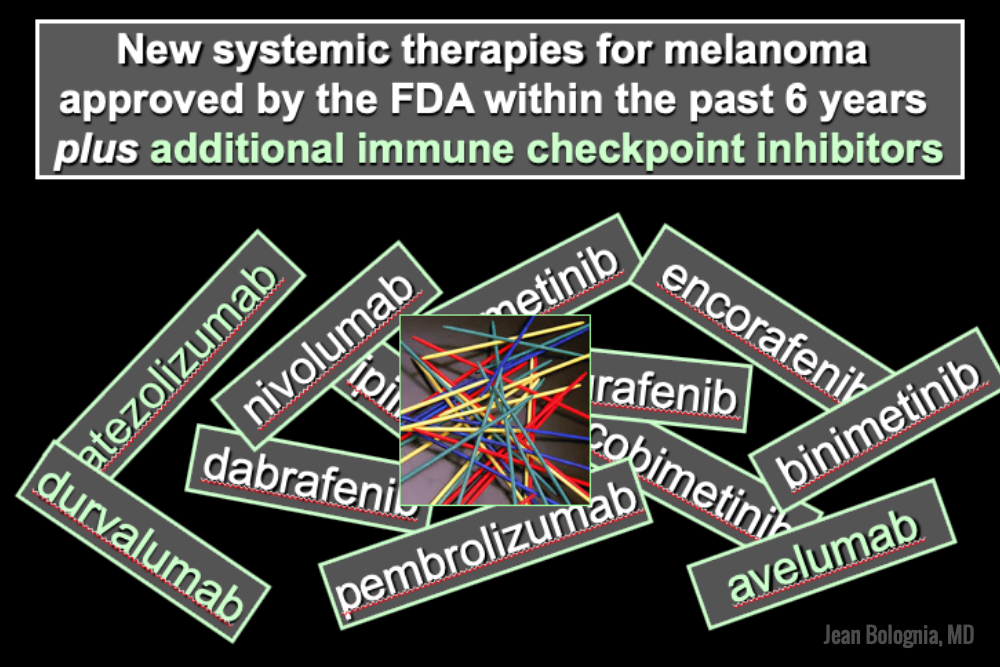
Source: Next Steps in Derm
This information was presented by Dr. Jean Bolognia at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL. The highlights from her lecture were written and compiled by Dr. Daniel Yanes, one of the 5 residents selected to participate in the Sun Resident Career Mentorship Program (a program supported by an educational grant from Sun Pharmaceutical Industries, Inc.). Dr. Yanes was paired with Dr. Jean Bolognia as his mentor.
The world of melanoma is evolving, and dermatologists need to be equipped with the knowledge to help their patients navigate this landscape. Newer therapies for patients with more advanced stages of melanoma have not only drastically improved survival, but we as dermatologists must be prepared to recognize and treat the cutaneous side effects of these medications. This is a brief summary of common systemic therapies for melanoma with which every dermatologist should become familiar.
Selective BRAF Inhibitors
Melanoma tumor cells often have activating mutations that lead to constitutive activation of the MAP kinase pathway (See figure). Such activation can then lead to unregulated cell growth and proliferation. The most commonly detected mutation in BRAF results in the substitution of glutamic acid (E) for valine (V) at the 600th position in the BRAF protein and is referred to as BRAF V600E. Selective BRAF inhibitors, e.g. dabrafenib, encorafenib and vemurafenib, specifically target altered BRAF proteins. You can easily recognize these medications from their names, with raf indicating they target (B)RAF and nib identifying them as inhibitors. They are administered orally and chronically and lead to rapid responses but unfortunately tumor resistance commonly develops, often within six months. There are cutaneous side effects that the dermatologist should recognize, including morbilliform and folliculocentric eruptions, UVA photosensitivity (e.g. vemurafenib), keratoacanthomas/squamous cell carcinomas, and changes in melanocytic nevi (eruptive, enlargement, involution).
MEK Inhibitors
When mechanisms of resistance to selective BRAF inhibitors were investigated, a common finding was re-activation of the MAP kinase pathway via activation of MEK, another kinase that is downstream from BRAF. MEK inhibitors, e.g. binimetinib, cobimetinib, trametinib, were then combined with selective BRAF inhibitors to reduce the development of tumor resistance. These drugs are identified by the presence of a -metinib suffix. Interestingly, compared to BRAF inhibitors alone, combination BRAF+MEK therapy is associated with significantly less, not additive, cutaneous side effects – a real benefit to the patient.
Immunotherapy is designed to stimulate the immune system to attack immunogenic melanoma cells. These monoclonal antibodies inhibit inhibitory signals that normally downregulate the immune system and thus act as immune checkpoints. These drugs model after the saying “the enemy of my enemy is my friend,” only it’s now “the inhibitor of the immune inhibitor is the immune stimulator.” CTLA4 is a receptor on regulatory T cells that plays an important role in diminishing immune responses. By blocking the inhibitory function of CTLA4 during the priming phase, the anti-CTLA4 antibody ipilimumab increases T cell immune activity. Peripherally, when the PD-1 receptor on T cells binds to its ligand, PD-L1, on tumor cells, an inhibitory signal results. In a similar fashion, the anti-PD-1 monoclonal antibodies approved for melanoma – nivolumab and pembrolizumab – can increase anti-tumor immune activity. Anti-PD-L1 monoclonal antibodies (e.g. avelumab, atezolizumab, durvalumab) have been approved to treat other malignancies, including Merkel cell carcinoma.

Source: Next Steps in Derm
This information was presented by Dr. Jean Bolognia at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL. The highlights from her lecture were written and compiled by Dr. Daniel Yanes.
Just as systemic lupus erythematosus (LE) can have protean systemic manifestations, cutaneous LE can present in many different ways. When confronted with the many faces of mucocutaneous LE, the following pearls can be valuable.
In 2012, the Systemic Lupus International Collaborating Clinics (SLICC) developed a set of clinical and immunologic criteria to assist in the diagnosis of systemic LE.
To meet criteria for systemic LE, a patient must fulfill at least four criteria, with at least one clinical criterion and one immunological criterion OR have biopsy-proven lupus nephritis in the presence of ANA or anti-dsDNA antibodies. Of the 11 clinical criteria, 4 are mucocutaneous: (1) acute or subacute cutaneous LE; (2) chronic cutaneous lupus; (3) non-scarring alopecia; and (4) oral or nasal ulcers. Of note, the dermatologist doesn’t just establish the diagnosis of cutaneous LE, but can also determine the specific types of autoantibodies the patient is forming as well as if the patient has systemic involvement (e.g. hematologic or renal abnormalities). Remember the latter requires a urinalysis in addition to bloodwork. Acute cutaneous LE is more closely associated with systemic LE than subacute cutaneous LE, which in turn is more closely associated with systemic LE than discoid LE. The cutaneous manifestations of LE per the SLICC classification scheme are as follows:
Acute cutaneous lupus
Subacute cutaneous lupus
Chronic cutaneous lupus
While ANA titer is positive in nearly all patients with systemic LE, not all patients with a positive ANA titer have LE.

Source: Next Steps in Derm
If you are navigating the confusing landscape of contract negotiations or considering partnership in a private practice after years of employment, then take note! Ron Lebow, Senior Counsel in the Health Law practice group at Greenspoon Marder LLP, led a fantastic workshop at the 2019 ODAC conference. He covered common concerns when negotiating employment agreements with dermatology practices, as well as issues to address when it comes time to become a partner.
The most important point and recurring theme of Ron Lebow’s workshop was simply this:
This point was stressed time and time again and will continue to be the overarching theme throughout the many parts of contract negotiations. With this in mind, here are some of the main takeaways and important questions we, dermatologists, should constantly keep in mind.
Surround yourself with experts! Find people who have your back. Make sure you find a lawyer who deals with medical professionals (particularly your specialty) for a living. You may need to find an accountant to work with you depending on your situation. Lastly, it may be in your best interest to work through recruiters. Some recruiters are better than others, and Ron Lebow recommends Dermatology Authority as an organization that provides good recruiting services for dermatologists.
When dealing with negotiations, it is important to recognize the many aspects of the process. With respect to the job you are offered:

Source: Next Steps in Derm
In a 20-minute lecture presented at the 16th Annual ODAC conference, Dr. Patel reviewed the appropriate management of actinic keratoses and squamous cell carcinoma. Grabbing the attention of the audience early on, Dr. Patel quoted the staggering statistics for squamous cell carcinoma – calling the growing epidemic “a public health crisis.” He challenged dermatologists to lead the charge in a more sophisticated approach to disease stratification.
Data are conflicting regarding the risk of progression of actinic keratoses to squamous cell carcinoma. Despite Dr. Patel’s expertise, he admitted even he finds it impossible to predict which lesions will progress. Instead, he takes a more astute approach and taking a step back to focus on the burden of disease.
With the groundwork firmly laid, Dr. Patel delved into the crux of his talk. He posed a thought-provoking question to captivated listeners: Are actinic keratoses a disease or a symptom? In the same way hypertension leads to stroke, actinic keratoses lead to squamous cell carcinoma.
Dr. Patel drove his point home with several instructive clinical cases. With each patient, Dr. Patel calls dermatologists to first discern field disease from invasive disease. Once invasive disease has been excluded, hyperkeratotic lesions should be debrided, and a strict regimen of topical 5-fluorouracil instituted for 4 weeks. This regimen should be followed by photodynamic therapy in 3 months.

Source: Next Steps in Derm
This information was presented by Dr. Susan Weinkle at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL. The highlights from her lecture and live demonstrations were written and compiled by Dr Nikhil Shyam.
Dr. Susan Weinkle, an expert in the field of aesthetic and surgical dermatology, shares important anatomical concepts to consider when using neurotoxins and fillers safely.
The face can be split into 3 zones – the upper 1/3rd, the middle 1/3rd and the lower 1/3rd. Knowing the important vessels and nerves in each zone as well as their corresponding depth in the skin is crucial in order to minimize injury and utilize a safe technique when injecting neurotoxins and fillers.
Figure 1: D corresponds to areas where deeper injections are safer to avoid vasculature and nerves. S corresponds to areas where superficial (intradermal injections) are safer to avoid vasculature and nerves. Vessels shown are cartoon depictions of some of the more common arteries including the supraorbital, supratrochlear, superficial temporal, facial and superior and inferior labial arteries. Also depicted are the supraorbital, infraorbital and mental foramen that are located along the medial limbus.

Source: Dermatology News
When caring for individuals with sun-damaged skin, dermatologists need comfort with the full spectrum of photo-related skin disease. From assessment and treatment of actinic keratoses (AKs) and field cancerization, to long-term follow-up of cutaneous squamous cell carcinomas (SCCs), appropriate treatment and staging can improve patient quality of life and reduce health care costs, Vishal Patel, MD, said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Actinic keratosis/squamous cell carcinoma in situ is not a disease; it’s a symptom of cutaneous carcinogenesis or field cancerization,” said Dr. Patel, director of cutaneous oncology at George Washington University Cancer Center, Washington. On the other hand, he added, “field disease can be a marker for invasive squamous cell carcinoma risk, and it requires field treatment.” Treatment that reduces field disease is primary prevention because it decreases the formation of invasive SCC, he noted.

Source: Next Steps in Derm
This information was presented by Dr. Adam Friedman at the 16th Annual ODAC Dermatology, Aesthetics and Surgical Conference held January 18th-21st, 2019 in Orlando, FL.
Dermatophytosis constitutes a big chunk of “bread and butter” in dermatology. In fact, an average of 4.1 million visits a year were due to dermatophytosis from 1995 to 2004! Nevertheless, these fungi can still stump the most seasoned dermatologist, and misdiagnosis can be surprisingly common. Dr. Adam Friedman, Professor, Interim Chair, and Program Director of Dermatology at George Washington School of Medicine and Health Sciences, recently presented interesting cases and practical pearls on how to diagnose and treat dermatophytosis. Here are some highlights.
Here’s the golden rule: if there is scale, scrape it! KOH preparation is first line in diagnosis of dermatophytosis. Do you follow this rule? A recent survey showed that the percentages of dermatologists who scrape when suspicious of dermatophytosis were only 20-30% (always) and 30-40% (very often). Next, histology can be helpful in diagnosing nail fungus and Majocci’s granuloma (where KOH is usually negative). Fungal culture be helpful to guide anti-fungal therapy, especially for tinea capitis in children.
Tinea Pedis
Tinea pedis is the most common form of skin fungal infection, and there are 4 types: moccasin, interdigital, bullous, and ulcerative.
Don’t forget that non-dermatophytes (S. dimidiatum; S. hyalinum) can cause identical findings! Also, an exuberant dermatophytid (or “id”) reaction, an inflammatory response to the fungal infection, can accompany findings of dermatophytosis. When you see a 2-hand-1-foot (or vice-versa) involvement, this can be another clue for diagnosing tinea pedis.
While topical azoles (econazole, other azoles) and allylamines (terbinafine, naftifine) and antifungal powder/spray weekly to shoes have been the mainstay treatment, there are some new topical options available. Luliconazole 1% cream (daily for 2 week) for moist macerated web space; naftifine 2% gel and cream (daily for 2 week) for dry, scaling plaques; and urea 40% cream for moccasin tinea pedis have shown efficacy.
What about systemic anti-fungal therapy? The moccasin type and vesicular type may warrant oral terbinafine 250mg BID for 2-6 weeks and 2 weeks, respectively. Since the vesicular type may have superimposed bacterial infection, an oral antibiotic may also be considered.
For more Tinea, click here.

Source: Practical Dermatology
Alan Menter, MD, has been awarded the Outstanding Researcher and Educator in Psoriatic Disease Award by the ODAC Dermatology, Aesthetics & Surgical Conference, in partnership with the Journal of Drugs in Dermatology (JDD).
The award recognizes Dr. Menter’s significant contribution and lifetime commitment to the advancement of psoriatic disease research as well as his work guiding the next generation of psoriasis experts and researchers.
“Dr. Menter has dedicated his career to improving psoriasis treatment options and standards of care while also pouring countless hours into up-and-coming psoriasis experts and researchers, ensuring his legacy will continue for generations to come,” said Shelley Tanner, CEO and president of SanovaWorks, which produces the JDD and ODAC.

Source: Dermatology News
The first time a man walks in for an aesthetic consultation, he probably doesn’t know what to expect, according to Terrence Keaney, MD, a dermatologist in private practice in Arlington, Va. And he may not even be sure what he’s looking for.
However, he probably knows what he doesn’t like about his appearance. When men are questioned, the three areas they are most concerned about is their hairline, their eyes, and their jawline, said Dr. Keaney, speaking at the Orlando Dermatology Aesthetic and Clinical Conference.
It’s important to evaluate men differently, not just for anatomic differences from women, but also for behavioral and psychological factors unique to men as aesthetic patients, he noted.

Source: Dermatology News
New tricks from ticks, near-zero Zika, and the perils of personal grooming: Dermatologists have a lot to think about along the infectious disease spectrum in 2019, according to Justin Finch, MD, speaking at the Orlando Dermatology Aesthetic and Clinical Conference.
Anaphylaxis from alpha-gal syndrome is on the rise, caused in part by the geographic spread of the Lone Star tick. Beginning in 2006, isolated cases of an anaphylactic reaction to cetuximab, the epidermal growth factor receptor antagonist used to treat certain cancers, began to be seen in a curious geographic distribution. “The anaphylaxis cases were restricted to the southeastern United States, the home of the Lone Star tick,” said Dr. Finch, of the department of dermatology at the University of Connecticut, Farmington.
With some detective work, physicians and epidemiologists eventually determined that patients were reacting to an oligosaccharide called galactose-alpha–1,3-galactose (alpha-gal) found in cetuximab. This protein is also found in the meat of nonprimate mammals; individuals in the southeastern United States, where the Lone Star tick is endemic, had been sensitized via exposure to alpha-gal from Lone Star tick bites.
“Alpha-gal syndrome is on the rise,” said Dr. Finch, driven by the increased spread of this tick. Individuals who are sensitized develop delayed anaphylaxis 2-7 hours after ingesting red meat such as beef, pork, or lamb. “Ask about it,” said Dr. Finch, in patients who develop urticaria, dyspnea, angioedema, or hypotension without a clear offender. Because of the delay between allergen ingestion and anaphylaxis, it can be hard to connect the dots.

Source:Dermatology News
When you extend your hand to a new patient, and he reflexively wipes his palm before shaking hands, be alert. It’s possible you’re seeing primary hyperhidrosis, a condition that’s both more common and more disabling than once thought.
“Looking at the biology of sweating, normally, it’s a good thing – we need it to survive. However, hyperhidrosis is too much of a good thing – it’s an excess of what is needed for normal biology,” said Adam Friedman, MD, speaking at the Orlando Dermatology Aesthetic and Clinical Conference.
Recent data, he pointed out, show that hyperhidrosis is more prevalent than previously thought – about 4.8% of individuals may have the condition, with about half having axillary hyperhidrosis. Symptoms peak in early adulthood, with adults aged 18-54 most affected. “These are the prime working years,” he said.
About 2% of teens are affected, and many adults report that symptoms began before they were 12 years old. Hand hyperhidrosis is a factor for computer and electronic device work, sports, and even handling paper and pencils, noted Dr. Friedman, professor of dermatology at George Washington University, Washington.
“Does it affect quality of life? Yes. We have data to support the impact. The adverse impact is actually greater than that of eczema and psoriasis,” he said, adding that patients won’t always bring up their concerns about sweating. “Often, it’s the patient who apologizes for having sweaty palms or who sticks to the paper on the exam table. It’s worth asking these patients if they are bothered by excessive sweating.”

Source: Dermatology Times
The Orlando Dermatology Aesthetic & Clinical Conference (ODAC), formerly known as Orlando Derm, is scheduled for January 18-21 at the JW Marriott in Orlando.
This year’s meeting will open with presentations from physicians who will address advances in treating skin of color, hot topics in surgical dermatology and cutaneous malignancy, the latest on photodynamic therapy, and a year in review from the Journal of Drugs in Dermatology, among others.
Drs. Eric Bernstein and Jason Pozner will host a panel discussion on “My Top Picks for Laser and Energy Based Treatments.” And, Dr. Joel Cohen will give an overview of facial arterial supply.
During the general session on Saturday, Jan. 19, Dr. Brian Berman will address managing urticaria, which will be followed by talks by Dr. Deirdre Hooper on platelet rich plasma for hair growth and skin rejuvenation; Dr. Andrew Alexis on keloids and disorders of hyperpigmentation in skin of color; and, Drs. Bernstein and Pozner will address advances in non-surgical skin tightening.
On Sunday, January 20, Dr. Jean Bolognia will open the day’s general session with a review of advances in systemic therapies for melanoma.
For more information, visit ODAC online at https://orlandoderm.org.

Source: Dermatology Times
Avoiding and treating vascular compromise with hyaluronic acid (HA) injections requires understanding the subtleties of underlying facial anatomy and keeping a well-stocked arsenal of treatments for impending necrosis, said an expert at the Orlando Dermatology Aesthetic and Clinical Conference (ODAC) in Miami.
“Some blood vessels may actually be in different locations than in some of the anatomic diagrams and cartoons that have long characterized their course,” said vice conference chair Joel L. Cohen, M.D., from Greenwood Village, Colorado, who serves on the teaching faculty for both the University of California, Irvine and the University of Colorado.
Although textbooks commonly depict the angular artery tracking adjacent to the nasofacial sulcus, he said, “it’s more common for the angular artery to be more lateral to that area, closer to the infraorbital distribution. In a recent cadaver study, only 19% of the time did the facial artery actually project upward along the side of the nose-cheek junction. But 32% of the time, the angular artery came off the facial artery earlier, and therefore coursed to more of the medial cheek area.”
The technique of aspirating before injecting is not foolproof. “There can be false negatives. A study indicates you probably have to pull back on the plunger for several seconds in order to physically be able to see if you’re in a vessel. We all surely realize that it is very difficult to have the needle in the exact spot you plan to inject, and then reposition your hand to pull back on the plunger of the syringe to try to aspirate, and then have your needle-tip remain in the exact same spot when you reposition again in order to inject. As you change your hand position to pull back on the plunger, you probably move a bit, maybe just a millimeter, from the original location to the location you later inject,” Dr. Cohen said.
A recent report also shows that it is possible to puncture and get into a vessel with small cannulas — the injectors aspirated blood despite using a cannula.

Source: Dermatology Times
Bringing more men into an aesthetic dermatology practice can expand the patient population, increase business revenue, and pay long-term dividends in terms of patient loyalty and repeat business.
But men aren’t like women when it comes to aesthetic concerns, so the strategies used to market your aesthetic offerings to female patients might miss the mark with men, cautioned Terrence Keaney, MD.
Men are less cosmetically savvy and need more upfront education and counseling, Dr. Keaney said at the 2018 Orlando Dermatology Aesthetic and Clinical Conference.
“I spend more time explaining therapies and what might be best for them,” he noted. “I explain the scientific rationale and treatment mechanisms so they will be more comfortable.” Making sure they understand is important, because “men often nod and don’t ask questions.”
The extra effort up front can pay off.
“The beauty of men is when they get a great result and are happy with you, men are very physician loyal. Once they get a great result, they’re yours forever,” said Dr. Keaney, an assistant clinical professor of dermatology at George Washington University, Washington, and a private practice dermatologist in Arlington, Va.
Cost is the leading deterrent for men to embrace aesthetic procedures, a factor that also ranks first among women. Men are also concerned that results will not look natural and want information about safety and side effects, Dr. Keaney said. “These deterrents can be overcome with proper education and counseling.”

Source: Dermatology News
Another reason not to prescribe opioids for postoperative pain – besides potentially adding to the epidemic the nation – comes from evidence showing these agents can impair wound healing.
In addition, epidermal sutures to close dermatologic surgery sites may be unnecessary if deep suturing is done proficiently. These and other pearls to optimize wound closure were suggested by Robert S. Kirsner, MD, PhD, professor and chair of the department of dermatology and cutaneous surgery at the University of Miami.
Avoid opioids for postoperative pain
“We know the opioid epidemic is a big problem. An estimated 5-8 million Americans use them for chronic pain,” Dr. Kirsner said at the Orlando Dermatology Aesthetic and Clinical Conference. “And there has been a steady increase in the use of illicit and prescription opioids.”
Emerging evidence suggests opioids also impair wound healing (J Invest Dermatol. 2017;137:2646-9). This study of 715 patients with leg ulcers, for example, showed use of opioids the most strongly associated with nonhealing at 12 weeks. “We found if you took an opioid you were less likely to heal,” Dr. Kirsner said. They found opioids significantly impaired healing, even when the investigators controlled for ulcer area, duration, and patient gender.

Source: Dermatology News
Pearls for providers of photodynamic therapy (PDT) include tips on skin preparation, eye protection, and use of three new codes to maximize reimbursement. Also trending in medical dermatology are best practices for intralesional injections of 5-FU to treat the often challenging isomorphic squamous cell carcinomas (SCCs) or keratoacanthomas on the lower leg, as well as use of neoadjuvant hedgehog inhibitors to shrink large skin cancer lesions, according to Glenn David Goldman, MD.
“This talk is about what you can do medically as a dermatologic surgeon,” Dr. Goldman said at the Orlando Dermatology Aesthetic and Clinical Conference.
Use new billing codes for photodynamic therapy
There are now three new PDT billing codes. “Make sure your coders are using these properly. They are active now, and if you don’t use them, you won’t get paid properly,” said Dr. Goldman, professor and medical director of dermatology at the University of Vermont, Burlington. Specifically, 96567 is for standard PDT applied by staff; 96573 is for PDT applied by a physician; and 96574 is for PDT and curettage performed by a physician.
“Be involved, don’t delegate,” Dr. Goldman added. “If you do, you will get paid half as much as you used to, which means you will lose money on every single patient you treat.”
What type of PDT physicians choose to use in their practice remains controversial. “Do you do short-contact PDT, do you do daylight PDT? We’ve gone back and forth in our practice,” Dr. Goldman said. “I’m not impressed with daylight PDT. I know this is at odds with some of the people here, but at least in Vermont, it doesn’t work very well.”
The way PDT was described in the original trials (a photosensitizer applied in the office followed by PDT) “works the best, with one caveat,” Dr. Goldman said. The caveat is that dermatologists should aim for a PDT clearance that approaches the efficacy of 5-fluorouracil (5-FU). “If you can get to that – which is difficult by the way – I think your patients will really appreciate this.”
An additional PDT pearl Dr. Goldman shared involves skin preparation: the use of acetone to defat the skin, even in patients with very thick lesions. Apply acetone with gauze to the site for 5 minutes and “all of that hyperkeratosis just wipes away,” curette off any residual hyperkeratosis – and consider a ring anesthetic block to control pain for the patient with severe disease, he advised.
Another tip is to forgo the goggles that come with most PDT kits. Instead, purchase smaller, disposable laser eye shields for PDT patients, Dr. Goldman said. “They work better. You can get closer to the eye … and they are more comfortable for the patient.”
Dr. Goldman’s practice is providing more PDT and much less 5-FU for patient convenience. “I believe if someone is willing to go through 3 weeks of 5-FU or 12-16 weeks of imiquimod, they get the best results. However, most people don’t want to do that if they can sit in front of a light for 15 minutes.”
Consider intralesional injections for SCCs and KAs on the legs
An ongoing challenge in medical dermatology is preventing rapid recurrence of SCCs and/or keratoacanthomas (KAs) near sites of previous excision on the legs. “We all see this quite a bit. Often you get lesions on the leg, you cut them out, and they come right back” close to the excision site, Dr. Goldman said.
He does not recommend methotrexate injections for these lesions. “Methotrexate does not work. It doesn’t hurt, but I’ve injected methotrexate into squamous cell carcinomas many times and they’ve never gone away.” In contrast, 5-FU “works incredibly well. They go away, I’ve had tremendous success. This has changed the way we treat these lesions.” 5-FU is inexpensive and can be obtained from oncology pharmacies. One caveat is 5-FU injections can be painful and patients require anesthesia prior to injection.

Source: Dermatology Times
Adam Friedman, M.D., was honored with the Innovations in Residency Training Award by the Journal of Drugs in Dermatology (JDD) at the Orlando Dermatology Aesthetic & Clinical Conference (ODAC) held in January. The award recognizes individuals who serve as exemplary role models for dermatology residents and innovate improvements in residency programs.
“Dr. Adam Friedman embodies the spirit of the award and more,” says Shelley Tanner, CEO and president of SanovaWorks, parent company of the JDD and ODAC. “He looks towards the future of dermatology and those who will carry it forward.”
Dr. Friedman is the residency program director and director of translational research at the George Washington University School of Medicine. He is also deputy chair of the American Academy of Dermatology’s Poster Task Force, senior editor of the Dermatology In-Review online workshop and cram pack, and director of the Oakstone Institute Dermatology Board Review.

Source: Dermatology Times
One of the only things the dermatology community knows about biosimilar use is that there are many unknowns. Still, biosimilars are on dermatologists’ radars as having the potential to lower the high costs of biologic treatments for chronic skin diseases, including psoriasis.
There also are misperceptions—even among dermatologists—about what biosimilars are and if these drugs can be used to treat patients, according to Leon H. Kircik, M.D., clinical associate professor of dermatology at Indiana University School of Medicine, Indianapolis; clinical associate professor of dermatology at Mount Sinai Medical Center, New York City; and medical director of Physicians Skin Care in Louisville, Ky. who presented “Biosimilars: What You Need to Know” at the Orlando Derm Aesthetic and Clinical conference in Miami, Fla., in January 2017.
Misperception number one
The first misperception is that biosimilars are generic biologics. They’re not, he says.
“You cannot have a generic of a biologic because every biologic is made differently. So, it is important for everybody to understand that biosimilars are not generics,” says Dr. Kircik,
As a result, the approval process for biosimilars is different for that of generics. Biosimilars came about because of the Biologics Price Competition and Innovation Act of 2009, which passed in Congress as a provision of the Affordable Care Act. Biosimilars have an abbreviated licensure pathway, but it’s a different pathway compared to a generic.
“Biopharmaceuticals are biopolymers of organic molecules that are manufactured in living systems. Function is based not only on the amino acid number and sequence but also on posttranslational modification (e.g. glycosylation) that are added by virtue of manufacture in living systems.”
Complexities and blurred lines
The FDA’s definition of a biosimilar, according to Dr. Kircik is, “A biological product that is highly similar to the reference product, notwithstanding minor differences in clinically inactive components. There are no clinically meaningful differences from the reference product in terms of the safety, purity, and potency”
“Those are very vague terms,” Dr. Kircik says.
The first biosimilar (not for use in dermatology), Zarxio [Sandoz], was FDA approved in March 2015. Zarxio is biosimilar to Neupogen (Amgen, filgrastim)1
More than a year later, the first biosimilar to have dermatologic indications received FDA approval—a biosimilar of infliximab, by the name of Inflectra (Celltrion). Interestingly, Inflectra, a biosimilar to Janssen Biotech’s Remicade, has an indication for psoriasis but no data on dermatologic disease, including psoriasis, Dr. Kircik says.

Source: Dermatology Times
Options for repairing nasal defects after skin cancer surgery should be based on location, size and depth of the defect, as well as patient preference.
“If the defect is centrally located in the alar groove, you may want natural healing to occur,” says Joel L. Cohen, M.D., associate clinical professor of dermatology at the University of Colorado in Denver, and director of AboutSkin Dermatology in Greenwood Village and Lone Tree, Colo. He spoke with Dermatology Times prior to his presentation on skin cancer nasal reconstruction at the recent Orlando Dermatology Aesthetic & Clinical Conference (ODAC) in Miami.
“In such a case, the natural concavity is often recapitulated by simply letting the skin granulate, without the need for any sutured repair.”
However, in many instances of nasal reconstruction, dermatologists have to decide which procedure will achieve the best aesthetic outcome and also, the level of wound care that can be managed by the patient.

Source: Dermatology News
In his practice, Joel L. Cohen, MD, spends a good part of his day doing Mohs surgery, “with the goal of cancer removal, and after surgery, having the patient look good,” he said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Having resurfacing in my practice has allowed me to treat not only wrinkles and etched lines, but also help skin cancer patients by blending and minimizing their skin cancer scars,” said Dr. Cohen, an aesthetic dermatologist and Mohs surgeon in private practice in Denver.
For example, one of his patients was a kindergarten teacher who had a large rotation flap scar on her cheek after excision of a melanoma in situ. The children asked her about it all the time during the 2 months after the surgery, and she decided to come in for some laser sessions. “With three ablative fractional laser sessions, she really looked great just 3 months later and wasn’t even interested in wearing makeup at that point.”
Resurfacing in his practice using a variety of lasers is very helpful, Dr. Cohen said. He published a study in November that compared pulse dye laser, CO2 ablative fractional lasers, or a combination of both for modification of scars following Mohs surgery (J Drugs Dermatol. 2016 Nov 1;15[11]:1315-9).
The prospective, multicenter study revealed that although both monotherapy approaches were safe and effective, the combination of pulse dye laser and fractional ablative laser offered some synergy that was preferred by patients.
Source: Dermatology Times
The FDA announced it has approved Eucrisa (Anacor Pharmaceuticals, crisaborole) ointment to treat mild to moderate eczema in patients two-years-of-age and older.
“We welcome this corticosteroid-sparing topical option,” says Elaine C. Siegfried, M.D., professor of pediatrics and dermatology at Saint Louis University, Cardinal Glennon Children’s Hospital, St. Louis, Mo. “The other two alternatives (pimecrolimus cream and tacrolimus ointment) carry black box warnings and labelled limitation on duration of use. Although most pediatric dermatologists prescribe these medications in infants and children without long-term safety concerns, prescribing Eucrisa is not hampered by this medicolegal burden. However, cost and access could be a limitation.”
Adam Friedman, M.D., associate professor of dermatology and director of translational research in dermatology at George Washington School of Medicine and Health Sciences, tells Dermatology Times that this most recent approval represents the exciting first of hopefully many new approved therapies for an exceedingly common disease state, which until recently was largely ignored.
“I envision crisaborole being used in a similar manner to calcineurin inhibitors, both as proactive treatment for affected delicate areas like the eyelids, face, body folds, groin or mild disease elsewhere. But, more importantly, [I envision it] as preventative maintenance therapy for disease areas that recur frequently after topical steroid use has been discontinued (though without the baggage of a black box warning and possible substance P induced burning at the onset of use),” he says.
Dr. Friedman, who is presenting on the topic of eczema at the January 16 to 19, 2017 Orlando Derm Aesthetic and Clinical conference in Miami, Fla., says this approval, however, should not overshadow the basic and requisite elements for properly managing this often chronic condition. These basics are: clear patient education on a broad range of topics, including realistic expectations; proper soap, moisturizer and treatment use; and myths about treatment safety, in order to gain the patient’s confidence, which in turn, increases the likelihood of regimen compliance, according to Dr. Friedman.

Source: Dermatology News
Tactics for managing patients with atopic dermatitis can go a long way to educate patients, set realistic expectations, and devise strategies for existing therapies, even as clinicians await some promising agents expected on the market soon.
“The good news is this is the Age of Eczema. In the last couple of years we’ve seen an explosion in the literature,” Adam Friedman, MD, of the department of dermatology, George Washington University, Washington, D.C., said at the Orlando Dermatology Aesthetic and Clinical Conference. Some of this research is spurring new therapeutics. a phosphodiesterase 4 inhibitor.
Crisaborole ointment, 2% (Eucrisa), a phosphodiesterase 4 inhibitor, was approved by the Food and Drug Administration in December 2016 for treating patients aged 2 years and older with mild to moderate AD, for example. It is a novel, nonsteroidal anti-inflammatory and the first prescription agent approved in the United States for atopic dermatitis in more than 10 years.
Dr. Friedman has no personal experience with crisaborole, which just became available. “But the data look encouraging. From what I’ve seen this may be a nonburning alternative to calcineurin inhibitors. It will be interesting to see how this will fit in our practices.”
