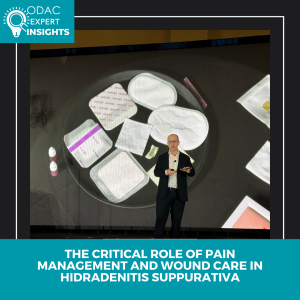
At the 2026 ODAC Dermatology Conference in Orlando, hidradenitis suppurativa (HS) expert Hadar Lev-Tov, MD, gave a high-yield, practice-focused lecture on two frequently underappreciated pillars of HS care: pain management and wound care. According to Dr. Lev-Tov, addressing these areas is essential to improving quality of life and overall outcomes for patients with HS.
Pain as a Core Component of HS Care
Dr. Lev-Tov emphasized that pain is not a secondary symptom of HS but a central driver of disease burden. A large proportion of patients experience moderate to severe pain, which often impacts quality of life more than objective disease severity. Despite this, pain remains underrecognized and undertreated in dermatology clinics. Because dermatologists serve as the primary physicians for most HS patients, Dr. Lev-Tov stressed that pain management must be viewed as an integral part of HS care. Uncontrolled pain also increases the risk of long-term opioid use, an association that persists even after adjusting for confounders.
A Multimodal, Bio-Psycho-Social Approach
To address chronic HS pain, Dr. Lev-Tov advocated for a multimodal strategy rooted in a bio-psycho-social framework. Pharmacologic management should follow a stepwise approach, beginning with topical or systemic NSAIDs and acetaminophen. For neuropathic pain, agents such as gabapentin, pregabalin, TCAs, and SNRIs (including duloxetine) may be effective. Short courses of tramadol or other short-acting opioids can be considered for acute breakthrough pain, with strict limits on quantity. Procedural interventions, such as intralesional triamcinolone or punch deroofing, and referral to pain specialists should be considered for refractory cases.
Equally important are non-pharmacologic therapies, which form the foundation of chronic pain management. These include physical activation strategies (physical therapy, yoga, low-intensity aerobic exercise), behavioral interventions (cognitive behavioral therapy and mindfulness), and adjunctive techniques (massage, acupuncture, and chiropractic care).
Wound Care: Small Details, Big Impact
The second half of the presentation focused on wound care, which Dr. Lev-Tov described as critical to patient comfort and daily functioning. While medical and surgical treatment address disease control, appropriate wound care can dramatically improve quality of life—and poor dressing choices can undermine even the best treatment plans.
Key pearls included selecting dressings based on wound depth and exudate level, with practical guidance on the use of foams, hydrocolloids, gelling fibers, calcium alginates, and superabsorbent dressings. Dr. Lev-Tov also highlighted evidence supporting wide excision with healing by secondary intent, noting excellent outcomes even for large HS wounds. Dedicated HS wound care systems, such as HidraWear, can further enhance comfort, confidence, and ease of use.
Additional surgical pearls included continuing biologic therapy through HS surgery, recognizing and managing hypergranulation tissue, and using chemical debridement, topical corticosteroids, or mechanical debulking when needed.
Takeaway
Dr. Lev-Tov’s lecture on pain management and wound care in HS reinforced that effective HS care extends beyond inflammation control. Pain management is essential—not optional—and thoughtful, individualized wound care plays a major role in improving patient quality of life. By embracing a multimodal pain strategy and a structured approach to wound dressing selection, dermatologists can make a meaningful difference for patients living with HS.
This session summary was written by Dr. Ryan Gall and published on Next Steps in Derm.