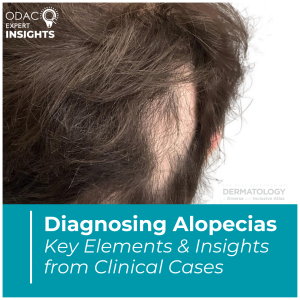
August is Hair Loss Awareness Month. At the 2025 ODAC Dermatology Conference, Ronda Farah, MD, FAAD, shared a comprehensive, systematic approach to diagnosing and managing hair loss, emphasizing clinical precision and patient-centered care.
Initial Evaluation: The “Top Ten” Checklist
Dr. Farah’s diagnostic approach begins within the first minute of the encounter by assessing:
- Scalp: For erythema, follicular signs, scaling, tenderness, and patterned thinning
- Hair shaft: For breakage due to chemical or heat damage
- Nails: For signs like pitting or trachonychia, which suggest alopecia areata or lichen planopilaris
- Eyebrows: For patchy loss, often seen in frontal fibrosing alopecia (FFA) or alopecia areata
Diagnostic Tools
She highlighted the value of non-invasive tools:
- Photodocumentation: An 8-image series to track progress and treatment response
- Hair pull/tug tests: To detect active shedding or fragility
- Hair mounts: To examine shaft abnormalities and growth phases
- Trichoscopy: To distinguish between scarring and non-scarring alopecias
- Scalp biopsy: For complex or unclear cases
Clinical Pearls from Real Cases
- Thorough scalp evaluation is essential: Localized hair loss may mask systemic or multifocal disease like alopecia areata or trichotillomania.
- Differentiate between androgenetic alopecia and CCCA: They may appear similar but show distinct trichoscopic features—miniaturization in androgenetic alopecia, and peripilar halos in CCCA.
- CCCA has systemic comorbidities: Genetic and fibroproliferative links suggest associations with type 2 diabetes, uterine fibroids, and breast cancer—prompting broader screening.
- FFA affects more than scalp: Look for eyebrow loss, facial papules, mucocutaneous changes, and even depressed frontal veins.
- Distinguish from traction alopecia, especially early in the disease course.
Cosmetic Considerations
- Hair loss affects self-esteem, driving interest in aesthetic treatments.
- Procedural caution in FFA: Avoid aggressive resurfacing in active disease due to impaired wound healing.
- Safer options: Non-ablative Nd:YAG laser for facial papules, oral isotretinoin, and carefully placed fillers to balance facial aesthetics.
- Be aware of rare complications like dermal filler-induced alopecia.
Conclusion
Dr. Farah emphasized that successful hair loss diagnosis and treatment requires a structured clinical framework, attention to subtle physical signs, and appropriate use of diagnostic tools. Her insights underscored the importance of holistic patient evaluation, inclusive of both physical and psychological needs. Mastery of these strategies leads to more accurate diagnoses, improved patient outcomes, and stronger provider-patient relationships.
This session summary was written by Dr. Damien Abreu and published on Next Steps in Derm.
