Source: Next Steps in Derm
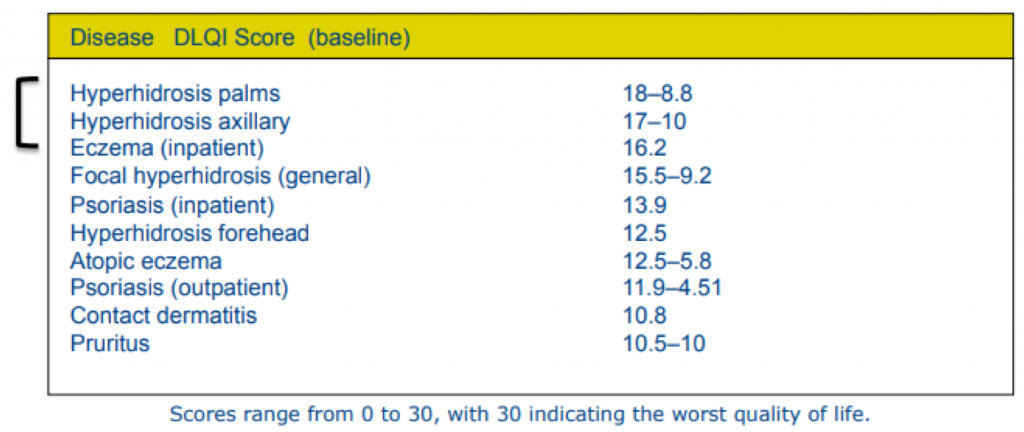
Can you think of a skin condition that has a greater negative impact on quality of life than eczema or psoriasis? That’s right, you guess it—hyperhidrosis! I still remember my first hyperhidrosis patient who refused to shake people’s hands, go on dates, or attend social events due to his condition. After his treatment, he was like a new man. I can’t tell you how satisfying it was to see his life changed after treatment. That’s why I’m so excited to share what I learned from Dr. Adam Friedman at ODAC 2019 regarding hyperhidrosis. Dr. Adam Friedman is Professor and Interim Chair of Dermatology, Residency Program Director, Director of Translational Research, and Director of the Supportive Oncodermatology Clinic in the Department of Dermatology at The George Washington University School of Medicine & Health Sciences.
Did You Know?
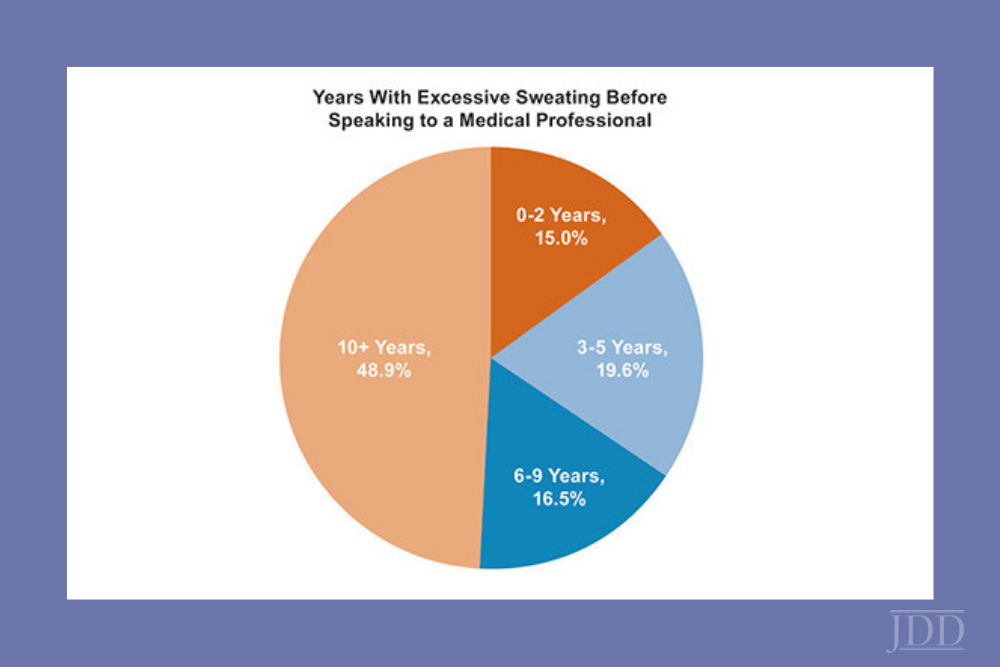
Nearly 5% of the world’s population suffers from hyperhidrosis—that’s 365 million people worldwide! In the U.S., 7.8 to 13.4 million people (2.8-4.8%) are estimated to be affected by hyperhidrosis—that’s comparable to the prevalence of psoriasis. Spalding et al. showed that patients with hyperhidrosis reported a worse quality of life compared to those with atopic dermatitis or psoriasis (Value in Health 2003). That made me raise my eyebrows for sure!
Know Your Sweaters: First, Diagnose
Hyperhidrosis can be divided into primary (usually focal) and secondary (generalized). For secondary hyperhidrosis, the underlying cause needs to be addressed, which may include drugs, cardiovascular disorders, respiratory failure, infections, malignancies, and metabolic disorders. For primary hyperhidrosis, now, that’s where we dermatologists step in and save the day. So, what are our options?
Treatment Options
There are non-invasive, minimally invasive, and surgical options for the treatment of hyperhidrosis. Here, we will discuss everything but surgical options and energy-based treatment.
- Topical aluminum chloride, aluminum chloride hexahydrate, or aluminum zirconium trichlorohydrex
- This is applied on skin overnight (to remain on skin for 6-8 hours, during non-sweating hours) and washed off in the morning before sweating begins
- A non-medicated deodorant should be applied in the morning after showering
- Can use topical steroids for skin irritation
- Cons: itching and burning of skin, time-consuming, can damage fabrics, temporary relief
- Inotophoresis
- Need treatment for 20-30 minutes a session, 3-4 times a week. This can be effective (81-91% response), but who has time for that?
- Cons: cumbersome, can be costly, long-term therapy, and again…time-consuming
- Topical glycopyrronium tosylate (Qbrexa)—the new kid on the block! And he’s FDA-approved, too. Whoohoo!
- This can be applied nightly onto clean skin and can be used in conjunction with an over-the-counter antiperspirant
- Improvement can be expected in 1-3 weeks.
- Can be used in kids (approved for >9 years of age)
- Cons: anticholinergic side effects such as dry eyes, dry mouth, blurred vision (need to emphasize the need to wash hands thoroughly after use to minimize risk), long-term therapy, may be costly
- Systemic anticholinergics: off-label use for hyperhidrosis
- Glycopyrrolate
- Can start at 1mg twice daily and increase up to 6mg a day, or until limited by anticholinergic side effects
- Oxybutynin
- Can start at 5 to 10mg daily and increase to 15 to 20mg daily
- A study in kids showed a 90% response rate at 2mg daily.
- Cons: again, anticholinergic side effects — ones listed above, as well as constipation, urinary retention, bradycardia, etc.
- Glycopyrrolate
- Beta-adrenergic blockers
- This is great for patients with social phobias and performance anxiety!
- Most can tolerate a dose of 10 to 20mg (to be taken 1 hour before). But don’t forget to check the resting blood pressure and heart rate beforehand! Oh, and also, they need a “test run” at home, just to make sure all goes smoothly before the actual “showtime”.
- Contraindications: bradycardia, AV block, asthma
- Botulinum toxin injection
- Before treatment: patients should avoid deodorants for 24 hours prior and rest comfortably for 30 minutes prior
- Treatment: after making an outline of the area, inject at a depth of 2mm, at a 45 degree angle with the bevel up, 1-2cm apart
- What to expect: onset is about 2-4 days and duration is 3-7 months
- Other considerations
- Topical analgesics help a ton!
- Do not use sterile water—can sting
- If you buy the toxin and inject, use the CPT code 64650 and J code J0585 (with units)
- If you prescribe the toxin to a pharmacy, provider bills only for the injection service, and patient pays co-pay for both the toxin and injections
- Cons: can be painful and expensive
