The ODAC Dermatology, Aesthetic & Surgical Conference (ODAC) recently announced changes to its advisory committee. Dermatologist Adam Friedman, MD, will now serve as ODAC co-chair. Dermatologist and Mohs surgeon James Spencer, MD, will now serve as ODAC co-chair emeritus.
Dr. Friedman, who has served as ODAC medical director since 2017, will now oversee ODAC’s medical dermatology offerings. He will serve alongside dermatologists and Mohs surgeons Joel Cohen, MD, who is co-chair of procedural dermatology, and Susan Weinkle, MD, who is co-chair of aesthetic dermatology. Dr. Friedman also is chair of the GW SMHS Department of Dermatology in Washington, D.C., and is the founding director of the GW Dermatology Residency Program, director of Translational Research in the Department of Dermatology and director of the Supportive Oncodermatology Program at the GW Cancer Center.
“Dr. Friedman has a wealth of knowledge on both medical dermatology and medical education, including how to create compelling educational experiences that translate into improved patient care,” said Shelley Tanner, CEO and president of SanovaWorks, which produces ODAC. “We look forward to his continued contributions for years to come.”
Dr. Spencer, who has served as ODAC chair for 10 years, will now serve as a senior advisor. He will also continue lecturing at ODAC on skin cancer related topics. Dr. Spencer is in private practice in St. Petersburg, Fla., and also serves as clinical professor of dermatology at The Mount Sinai School of Medicine in New York.
“Dr. Spencer has been instrumental in ODAC’s growth since the conference’s inception,” said Ms. Tanner. “We are grateful for his leadership and look forward to his continued impact through his advisory role.”
ODAC, which was founded in 2003, historically attracts nearly 800 dermatology physicians and allied health professionals each year. The 2022 event will take place January 14-17 at the Rosen Shingle Creek in Orlando.

New York (Mar. 17, 2021) – Adam Friedman, MD, medical director of the ODAC Dermatology, Aesthetic & Surgical Conference (ODAC) was recently named chair of the GW SMHS Department of Dermatology in Washington, D.C. Dr. Friedman has served as interim chair since February 2019, and is the founding director of the GW Dermatology Residency Program, director of Translational Research in the Department of Dermatology and director of the Supportive Oncodermatology Program at the GW Cancer Center.
During his time as interim chair, Dr. Friedman further strengthened collaborative ties between ODAC and GW SMHS through multiple and ongoing educational activities, including the GW Translational Science Lecture Series, the award-winning Krazy Kodachromes, and more recently, the 2020 DCAD conference, the GW Appraisal of Acne conference and the Core Crusher Basic Boot Camp Exam Prep Course.
“Dr. Friedman has worked tirelessly to ensure all dermatologists have access to the latest educational developments in the specialty,” said Shelley Tanner, CEO and president of SanovaWorks, which produces ODAC. “He expertly knows how to engage audiences in their education, creating programs that make learning compelling and applicable to daily practice. We are thankful to have his insight at work in our programs.”
Dr. Friedman has served as ODAC medical director since 2017. In this role, Dr. Friedman has been instrumental in cultivating and expanding the medical dermatology section of the educational program, in addition to generating opportunities for residents.
Dr. Friedman also serves on the editorial board of the Journal of Drugs in Dermatology (JDD), hosts the JDD Podcast and is the senior editor of and chairs the Derm In-Review Advisory Council. JDD and Derm In-Review are also products of SanovaWorks.
ODAC, which began in 2003, historically attracts nearly 700 dermatology physicians, residents, nurse practitioners and physician assistants each year. The 2022 event will take place January 14-17 at the Rosen Shingle Creek in Orlando.
###
Source: Next Steps in Derm
What is Hyperhidrosis (HH)?
Primary HH is defined as excessive, bilateral, and generally symmetrical sweating at abnormal levels unprompted by activity or environment.
Hyperhidrosis is characterized by abnormal sweating beyond what is needed for thermoregulation. It is not a normal physiologic response. Nearly 15 million people in the United States suffer from hyperhidrosis and half of those individuals have axillary hyperhidrosis. HH peaks in adulthood and approximately two-thirds of these individuals have never discussed their primary axillary hyperhidrosis with a healthcare professional.
Why aren’t more patients seeking help for their abnormally excessive sweating?
Many of these patients do not realize their excessive sweating is a medical condition and are unaware of protentional treatment options. On average, patients wait at least 10 years before seeking medical help for their abnormally excessive sweating1.
Patients with hyperhidrosis are reluctant to seek medical care, despite the negative impact on their quality of life.
Primary versus Secondary Hyperhidrosis
Primary Focal Hyperhidrosis is defined as excessive focal sweating of at least 6 months duration without any obvious cause with at least two of the following features:
-
- Onset before age 25, often as early as 9 years old
- A bilateral and symmetric pattern
- Impairment of daily activities
- Occurring at least once per week
- Cessation during sleep
- A positive family history
90% of all diagnosed cases of HH are primary and two-thirds of all HH patients report a positive family history.
Secondary Generalized Hyperhidrosis can be caused by or associated with another medical condition or results as a side effect of a medication. It usually presents with large areas of the body affected. Patients with secondary HH may experience sweating even when they are sleeping. It is important to differentiate between primary and secondary hyperhidrosis. Review the patient’s medical history and review of systems should point to any secondary causes. Patients who do not fit the classic pattern of primary hyperhidrosis should undergo further evaluation, and may need laboratory studies or radiographic evaluation.
Can the coronavirus spread through sweat?
There is no evidence that Covid-19 can be transmitted through sweat. The virus is transmitted by respiratory droplets. Dr. Adam Friedman notes that sweat could actually help prevent the transmission of Covid-19 due to the inherent antimicrobial activity of sweat. For anyone worried about transmission of the virus, it’s important to emphasize key tenets voiced from experts:
-
- Wash/sanitize your hands often and well
- Avoid touching your face
- Wear a mask in public
- Maintain physical distance, about 6 feet, from others
- Sanitize frequently-touched surfaces
- Follow your community’s public health recommendations
For more information, visit the International Hyperhidrosis Society’s (IHS) website: www.sweathelp.org
IHS is the only independent, non-profit, global organization that strives to improve quality of life among those affected by hyperhidrosis.
Treatment of Hyperhidrosis
A wide range of techniques has been utilized in the treatment of HH. First-line therapy for HH is topical formulations. Over-the-counter antiperspirants are usually not strong enough to significantly improve excessive sweating. Prescription aluminum salts are usually the first-line treatment for HH. The aluminum salts act as a plug, precipitating and blocking the sweat ducts. Sweating is reduced in the evening. Thus, application to dry body surfaces at night is ideal. Non-medicated deodorant can be applied in the morning after bathing. The fragrance from deodorants can be used to mask body odor from the microbiome of the skin.
Topical Aluminum Pearls:
-
- Aluminum salts must remain on the skin for 6 – 8 hours to be effective
- Overnight application is recommended
- Wash treated skin in the morning before sweating begins
- Wait 24 to 48 hours after shaving
- Beware of damage to fabrics
- A reaction occurs when aluminum mixes with the salts of your sweat, which may cause yellow stains on white fabrics.
- Irritated skin can be treated with low potency topical steroid
- Aluminum salts must remain on the skin for 6 – 8 hours to be effective
Topical antiperspirants are just not that effective for hyperhidrosis.
While over-the-counter products are most commonly recommended, they offer the least patient satisfaction. Topical antiperspirants are safe and simple to use. However, application is time-consuming, only provides temporary relief, and may cause skin irritation at the application site.
Fortunately, there are novel topical therapies available to patients with excessive underarm sweating, or axillary hyperhidrosis. Topical glycopyrronium tosylate (GT) wipes are FDA approved for treatment of axillary HH. This is the first and only prescription cloth towelette approved to treat excessive underarm sweating. GT works by blocking receptors responsible for sweat gland activation1. A significant number of patients can see improvement as early as 1 week. After 4 weeks of treatment in the clinical trials, GT resulted in substantially greater improvements compared to the control group. Patients were happy with the fast onset of effect and reported overall improved quality of life2:
-
- No longer avoiding interactions with other people
- No longer showering/bathing more than once a day or changing shirts during the day
- Feeling less embarrassed or confident
- No longer avoiding activities for work or hobby
Topical Glycopyrronium Tosylate Pearls:
-
- Approved for use in children ≥9 and adults
- Applied nightly to clean axillary skin
- Use 1 towelette by wiping across each entire underarm once
- Wash hands thoroughly after use to avoid inadvertent transfer of the drug to areas such as the eyes
- No need to remove hair or occlude the area for use
- May use OTC antiperspirants as needed
- Most patients see improvement by 2-3 weeks
- May hold dose as needed
Dr. Friedman notes that use of topical GT for treatment of palmar/plantar hyperhidrosis is off-label. He instructs his patients to rub the towelette between hands until dry, apply Aquaphor, and then wear gloves for at least 1 hour, in order to achieve clinical benefits.
It is important to monitor for anticholinergic side effects. The most common reported adverse effects include dry mouth and mydriasis. Use of gloves with the towelette and careful handwashing can help mitigate anticholinergic side effects. GT is non-invasive, effective, and well-tolerated. There is minimal irritation and can be safely used in pediatric populations. Aside from long-term therapy and potential for cost issues, topical GT provides clinically meaningful benefits for patients with primary axillary hyperhidrosis.
Iontophoresis
Iontophoresis is a process of transdermal drug delivery by use of a voltage gradient on the skin. It is often recommended for patients who have failed topical therapies or in patients with HH of the palms and soles. During iontophoresis, a medical device is used to pass a mild electrical current through water and through the skin’s surface1. Aluminum chloride or anticholinergics can be added to the water to help draw electric current. This non-surgical method is painless and effective. However, it requires long-term, weekly therapy to maintain efficacy. Of note, iontophoresis is contraindicated in patients with pacemakers or implants, or during pregnancy.
Microwave device
Non-invasive microwave technology uses thermal energy to ablate sweat glands. The device is FDA approved for treatment of severe axillary HH. The treatment is performed in a physician’s office with local anesthesia. Patients typically require 1-3 treatments to achieve long-lasting results. There is little to no discomfort during the procedure. Side effects are minor and include underarm swelling, redness, and tenderness lasting for several days. Numbness and tingling can occur in the upper arm or armpit and may last for about 5 weeks1.
Systemic Therapies
There are no systemic agents FDA approved for treatment of HH. Most data for systemic treatment comes from case reports or small case series. Systemic treatment may be more helpful in multifocal hyperhidrosis or hyperhidrosis of spinal cord injury. The two most common prescribed oral agents include Glycopyrrolate and Oxybutynin.
Glycopyrrolate does not cross the blood-brain barrier, resulting in less CNS effects. There is also an oral solution available for pediatric populations. Oxybutynin is safe in children as well. These therapies are cost-effective, but long-term therapy is required.
-
- Adverse effects due to Anticholinergic properties:
- Dry mouth
- Dry eyes
- Constipation
- Blurred vision
- Difficulty with urination
- Adverse effects due to Anticholinergic properties:
There is a risk of hyperthermia in pediatric patients taking systemic anticholinergics. It is important to watch for behavioral changes, as well as drowsiness, dizziness and confusion. Despite the efficacy, most patients discontinue therapy due to anticholinergic side effects.
Other systemic therapies include beta-blockers and Clonidine. Beta-blockers can be used for social phobias/performance anxiety. However, it is contraindicated in patients with bradycardia, AV block, or asthma. Of note, beta-blockers are a common cause of drug-induced psoriasis or exacerbation of psoriasis. Consider other treatment options in patients suffering from both psoriasis and HH. Clonidine has been evaluated in small case series. It is a great medication in treating patients with both hyperhidrosis and flushing.
Minimally invasive approaches
OnabotulinumtoxinA is FDA approved for axillary hyperhidrosis unresponsive to other therapies. It prevents release of acetylcholine from the neuromuscular junction. Injection technique involves a grid pattern (mapped via surgical marker) using a 30-gauge needle. Injection depth is approximately 2 mm and at a 45º angle to the skin surface with bevel side up. Injections are spaced 1-2cm apart for a total of 50 units injected per axilla.
Click here to view the full poster PDF.
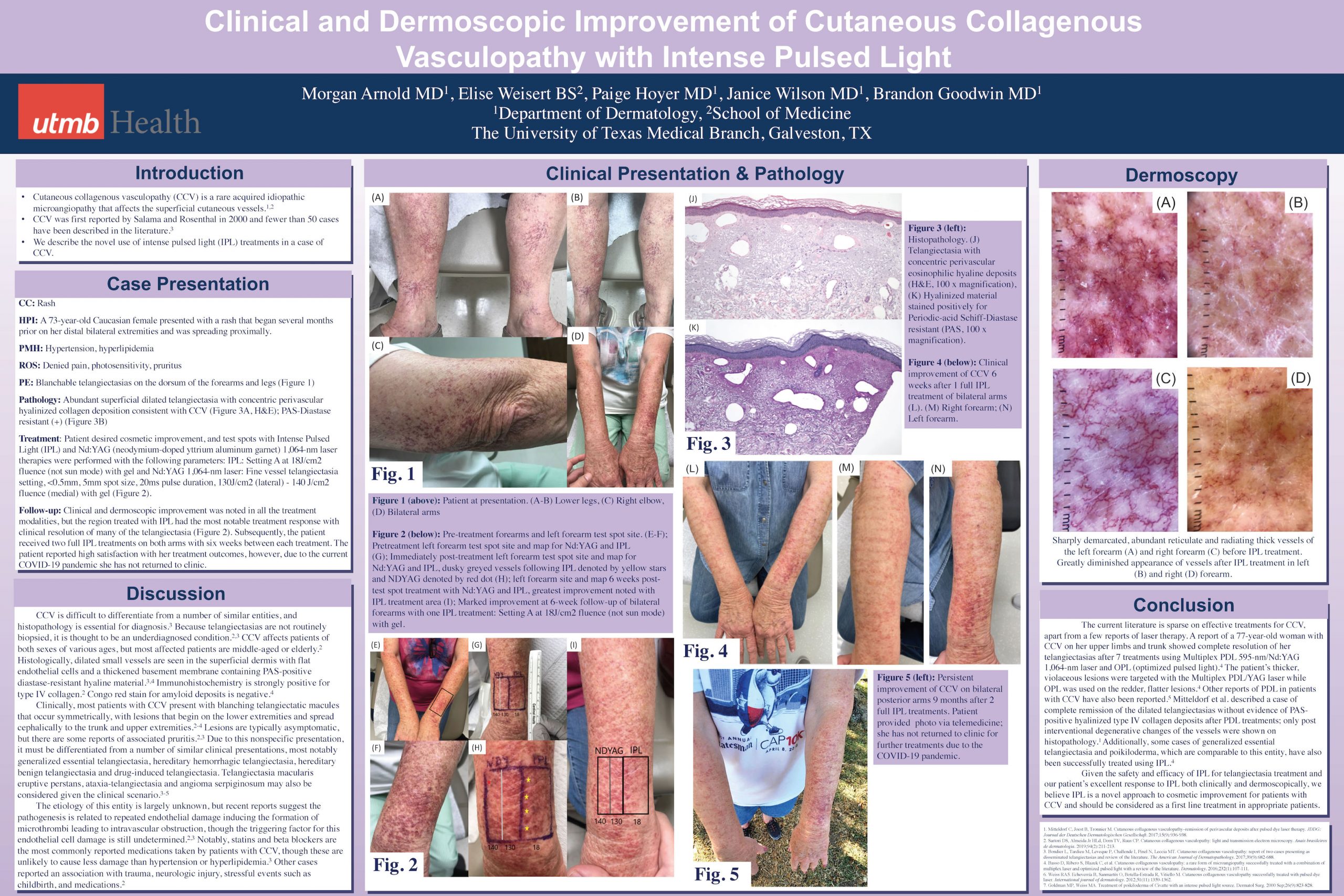
The following poster was presented at the 2021 Virtual ODAC Dermatology, Aesthetic & Surgical Conference.
Authors: Morgan Arnold MD, Elise Weisert BS, Paige Hoyer MD, Janice Wilson MD, Brandon Goodwin MD
Cutaneous collagenous vasculopathy (CCV) is a rare acquired idiopathic microangiopathy that affects the superficial cutaneous vessels. We describe the use of intense pulsed light (IPL) treatment in a case of CCV resulting in clinical and dermoscopic improvement. A 73-year-old Caucasian female presented with a rash on the arms and legs spreading proximally. Histopathology revealed abundant superficial dilated telangiectasia with concentric perivascular hyalinized collagen deposition and hyalinized material stained positively for Periodic-acid Schiff-Diastase resistant, confirming a diagnosis of CCV. Intense Pulsed Light (IPL) and Nd:YAG (neodymium-doped yttrium aluminum garnet) test spots were performed, with marked improvement with IPL therapy on follow-up. Two subsequent full IPL treatments were performed on patient’s bilateral arms, exhibiting significant clinical and dermoscopic improvement. Though effective treatments for IPL are scarce in the literature, there are reports of treatment with Multiplex PDL 595-nm/Nd:YAG 1,064-nm laser and optimized pulsed light. Furthermore, comparable entities to CCV such as generalized essential telangiectasia and poikiloderma have also been shown to be successfully treated with IPL. We present the use of IPL for successful cosmetic therapy in a patient with CCV.

For most dermatologic conditions, my mantra for treatment tends to be “less is more”. I prefer to use the fewest number of creams, pills, and steps to achieve the best results. However, after watching this year’s ODAC Sneak Peek Inflammatory Diseases Symposium, I may have a new mantra for treating my rosacea patients – “forks, spoons, and knives”.
At the ODAC 2021 Pre-Conference Sneak Peek Inflammatory Diseases Symposium, Dr. Julie Harper, dermatologist at the Dermatology and Skin Care Center of Birmingham and Founding Director of the American Acne and Rosacea Society, built a case for use of combination therapy for rosacea. It is well known that there are four subtypes of rosacea – erythematotelangiectatic, papulopustular, phymatous, and ocular. However, most patients don’t fall into one subtype, but rather, many experience subtype overlap. This is why Dr. Harper believes that clinicians should “start subtyping lesions” and treat all the lesions that are observed, even if that means use of multiple therapeutic agents.
Not only are there multiple targets clinically, but treatment for rosacea can also be targeted on a cellular level. The role of innate immunity including cathelicidins, specifically LL-37, and toll-like receptor 2 induction via demodex has been described in the pathogenesis of rosacea. But did you know that many of the well-known triggers of rosacea such as heat, stress, exercise, and spice have been implicated to affect rosacea on a cellular level? I certainly didn’t! Dr. Harper explained that common triggers of rosacea cause neurogenic inflammation via induction transient receptor potential channels to release substance P and calcitonin gene-related peptide, which cause vasodilation.
Forks, Spoons, and Knives
To better understand therapeutic options, Dr. Harper compares the various treatments to utensils, categorizing them into forks, spoons, or knives. She states that treating rosacea is like eating a meal – you can’t get by with just one utensil. While a spork would be a plausible loophole to this one-utensil-meal challenge, we don’t quite have a spork for treating rosacea (yet!). So what exactly are the utensils that Dr. Harper explained?
Forks are medications that treat papules and pustules, including:
-
- Ivermectin
- Metronidazole
- Azelaic acid
- Sodium sulfacetamide/sulfur
- Modified release doxycycline
Spoons should be utilized for persistent background erythema, such as:
-
- Brimonidine
- Oxymetazoline
Finally, knives are device-based treatments:
-
- Pulsed dye laser
- KTP
- IPL
- Electrosurgery
Why Combination Therapy?
Before showing us the evidence that combination therapy works, Dr. Harper described the goals of combination therapy:
-
- Achieve clear skin
- Achieve treatment goals more quickly
- Maximize remission periods
- Minimizing burden of disease
First, she reviewed a JDD article (Fowler J. J Drugs Dermatol. 2007;6(6)641-646) that combined two forks: modified release doxycycline and metronidazole gel. This 16-week study compared combination modified-release doxycycline with metronidazole 1% gel to metronidazole 1% gel with placebo. Metronidazole was discontinued at week 12 and doxycycline or placebo continued through week 16. At week 4, patients who received combination therapy had greater reduction of inflammatory lesion counts and were generally better faster. Then after week 12, those who continued on modified release doxycycline had better sustained results.
Next, Dr. Harper reviewed another JDD study (Stein Gold L, Papp K, et al. J Drugs Dermatol. 2017;16(9):909-916) that combined a fork and a spoon – ivermectin and brimonidine – to treat both moderate to severe erythematotelangiectatic and papulopustular rosacea. Three groups were identified in this study – one receiving vehicle only, one receiving ivermectin for 12 weeks with addition of bromonidine at week 4, and one receiving both ivermectin and brimonidine for 12 weeks. The most striking result from this study was that those who used combination therapy for 12 weeks had double the rate of improvement of redness in the three hours after brimonidine use. Dr. Harper explained that despite the use of a really good fork (ivermectin), there was still enough residual redness that the spoon (brimonidine) could make a meaningful impact. Thus, targeting inflammation and pustules alone will not lessen background erythema.
Learn what integrated skin care is and how to incorporate skincare to compliment your in-office procedures. All US-based practitioners that attend the full webinar, will receive a 30 mL CE Ferulic!
Date: Tuesday, December 8, 2020
Time: 7:00 – 8:00 PM ET
Faculty: Sheila Barbarino, MD, FACS, FAAO, FAACS
The American Academy of Dermatology (AAD) 2021 has announced the cancelation of the annual meeting in March.
On November 23, 2020, a message was sent to all Academy members and all attendees registered for the 2021 Annual Meeting schedule for March 19 – 23, 2021 in San Francisco, California.
Like ODAC Dermatology Aesthetic and Surgical conference, the health and safety of attendees, faculty, and sponsors comes first. Given the current situation with the pandemic, ODAC is committed to providing high-quality education in an engaging virtual format with top speakers and important topics.
Although we will miss seeing everyone in person at ODAC and the AAD 2021, we aim to provide a unique virtual experience that will continue to drive dermatology education and networking forward.
Experience ODAC virtually thought the free sneak peek Dec, 3rd, Resident Week Jan 8th and the full conference ODAC Jan. 14th. ODAC offers a unique 100% live experience. ODAC is not pre-recorded, offering hours of panels, CME, live polling and an enhanced attendee experience.
NEW YORK, (June 3, 2020) – Shelley Tanner, SanovaWorks (parent company of ODAC) CEO/President
The below was sent to the employees of SanovaWorks.
This is an issue we should all be aware of, we should all be engaged in, and we should all be actively fighting together against for a solution. Each company, as a collective of humans, has a responsibility to do everything we can to protect our fellow humans and ensure that we all have access to the things we hold dear. We cannot stand by knowing that our fellow Americans are being targeted unjustly from all angles.
On the heels of the global and national devastation of the coronavirus pandemic, we are witness to the glaring evidence of an epidemic that has existed for hundreds of years in the USA, and that is the systematic racism and injustice against black Americans. The devastation that results from this affects lives in literally every facet: education, careers, health, families, finances, safety, etc.
The pandemic unveiled in clear numbers the disparity between black and white communities in this country, where only 13% of the population are African American, yet represent 23% of the deaths. In some states, like Georgia, African Americans make up little more than 30% of the population, yet almost 50% of deaths are from within this group.
On May 25th this year George Floyd, a black man from Minneapolis who is also a brother, a cousin, a nephew, a friend, a boyfriend, a son, and a fellow human, was murdered in a horrific incident that has reinvigorated people to stand up and say that this is not acceptable, spurring the nationwide protests that are not only just, but also necessary to demand change for a reality that has been accepted through complacency and inaction.
What can we do?
For our employees who are impacted by this, we need to support you. As a team and your friends we are here to back you up.
If you don’t already know how you can personally help, I hope you will take the time to learn what we can all be doing at this time to be a part of the solution. You might feel helpless or overwhelmed by this matter, and feel like there is nothing you can do, but this is part of the problem. Doing nothing is a choice and an action. The support we show for one another matters. One of my friends sent me this article on the weekend, for which I was extremely grateful, as it outlines many things we can all be doing for racial justice.
READ What White People Can do for Racial Justice
President Barack Obama
On June 1, President Obama published an article on how he believes we can use what is happening now as a turning point for real change that is definitely worth the read. In this article there is a link to a very detailed report and toolkit developed while he was in office by the Leadership Conference on Civil and Human Rights, along with a dedicated site of resources and organizations to learn about and get involved with.
READ How to Make this Moment The Turning Point for Real Change
Grassroots Organizations
Below is a list of grassroots organizations supporting this cause. I have personally donated, and I encourage you all to consider doing the same. There are many more that I have read about and perhaps that speak to you more personally. I encourage you to look up some of these groups and read about what they are doing.
https://minnesotafreedomfund.org/
https://www.blackvisionsmn.org/
https://www.reclaimtheblock.org/home
https://www.northstarhealthcollective.org/
On Wednesday June 3rd
We as a company will take a moment of silence at 1:30pm ET to reflect on these injustices, and how we personally might help. I would like us all to pause together and show solidarity. For those who choose to sit on their own, know we are with you.
I am committed to ensuring that this is not the end of the conversation for SanovaWorks. Stay tuned for more information and please get in touch with me directly if you have thoughts on this. I welcome all ideas and feedback.
And finally. To ALL of our friends of color: know that we see you, we appreciate you, and we will do everything we can to support you.
Shelley N. Tanner
President/CEO